Session Information
Session Type: Abstract Session
Session Time: 3:00PM-4:30PM
Background/Purpose: Dermatomyositis (DM) is often misdiagnosed due to its diverse clinical presentation. This study aimed to identify common dermatologic mimics of DM, characterize misdiagnosis rates across inflammatory skin disease (ISD) subgroups, evaluate distinctions between myopathic DM and amyopathic DM (ADM), and describe histopathologic findings associated with misdiagnosed cases.
Methods: This single-center retrospective cohort study from the Johns Hopkins Myositis Center included patients with DM, queried using ICD-9/10 codes (710.3/M33.10), and ≥1 dermatology visit between 2005-2023. Patients with juvenile DM or mixed connective tissue disease, as well as those not meeting the ACR diagnostic criteria, were excluded.
Electronic medical records were reviewed to collect patient demographics, DM subtype (e.g., myopathic and ADM), and DM-associated comorbidities. Dermatology records were reviewed to identify all dermatologic diagnoses, and corresponding EpicTM diagnoses were extracted and classified into 1 of 40 dermatologic disease groupings, with 16 groups determined to be ISDs.
The identification of potential misdiagnoses was a central study element. Instances in which the ISD diagnosis occurred after the DM diagnosis were considered true co-diagnoses. ISD diagnoses preceding DM diagnosis were considered misdiagnoses if explicitly labeled as such by the dermatologist or if present until DM confirmation and absent in all follow-up visits, accounting for clinical and anatomical context through manual chart review. Skin biopsies in patients with misdiagnoses were documented.
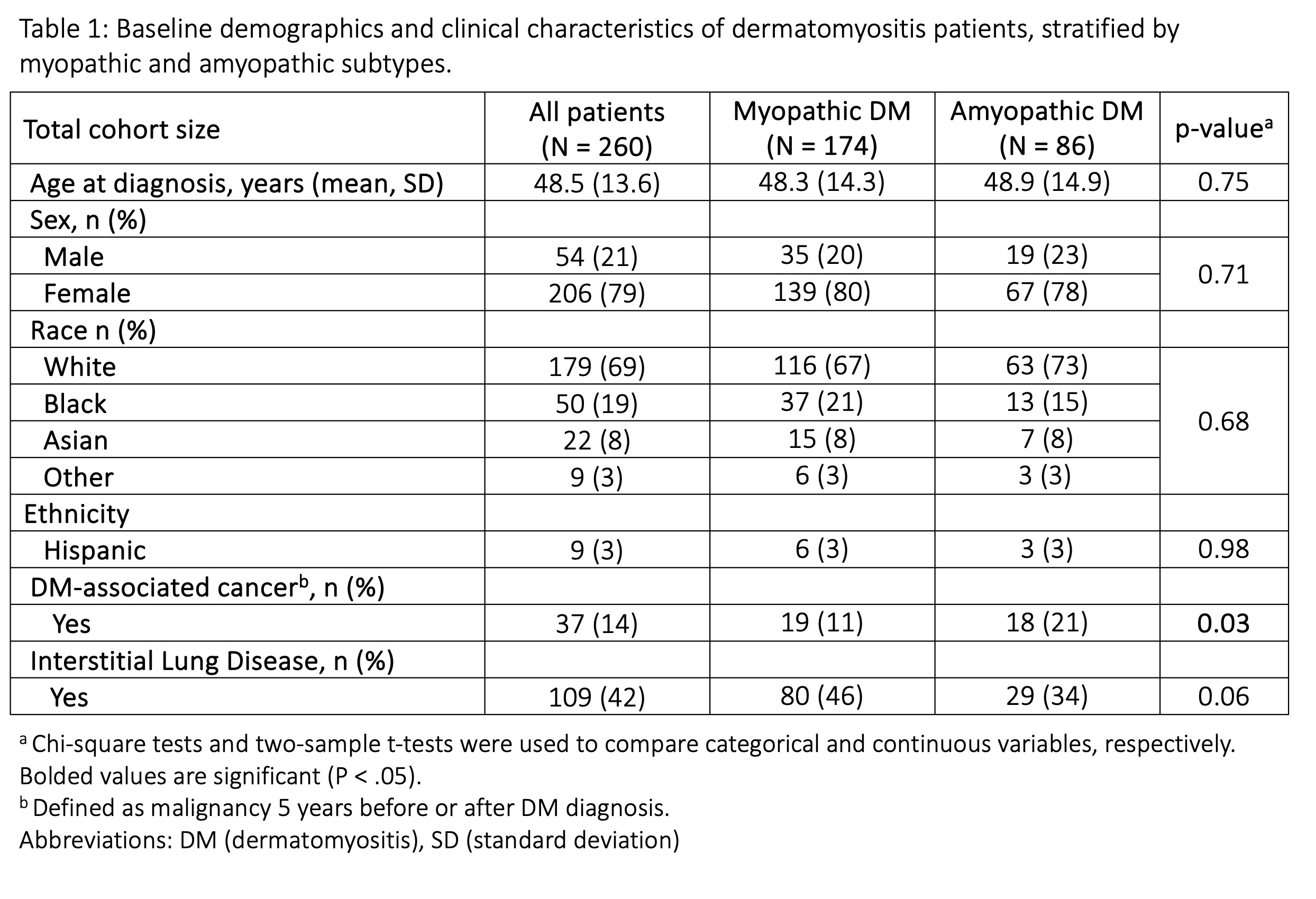
Results: 260 patients were included in the study, and 86 (33.1%) patients had ADM. The ADM cohort had higher rates of malignancy (20.9% vs 10.9%; p = 0.03), whereas the myopathic DM cohort had higher rates of ILD, although not statistically significant (46.0% vs 32.6%; p = 0.06).
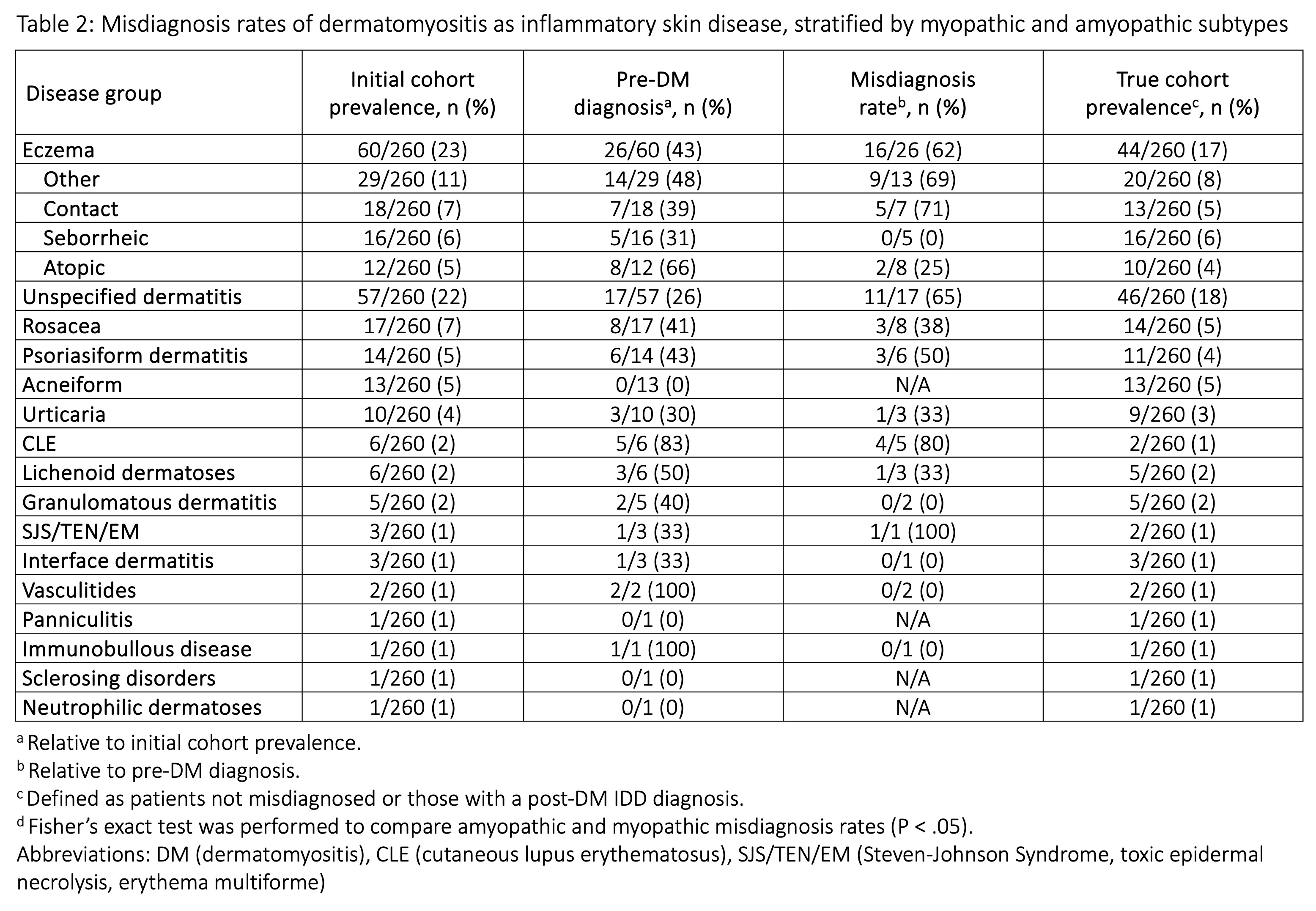
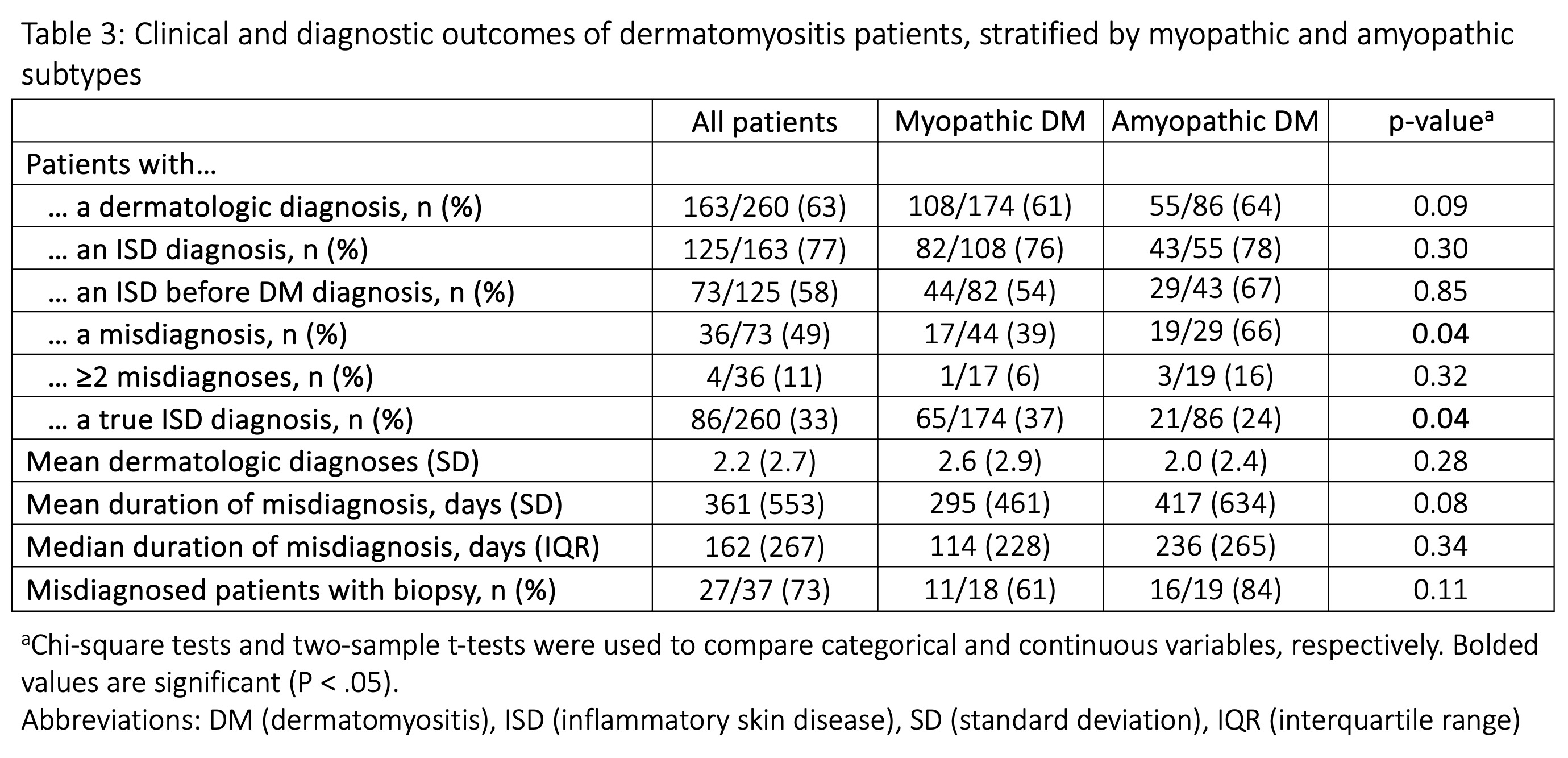
163 (62.7%) patients had ≥1 dermatologic diagnosis, of which 125 (77%) had an ISD. The most prevalent ISD were eczema (23.1%), unspecified dermatitis (21.9%), rosacea (6.5%), psoriasiform dermatitis (5.4%), and acneiform dermatitis (5.0%). 73 of 125 (58.4%) patients had an ISD diagnosis prior to their DM diagnosis. Of these, 36 (49.3%) experienced misdiagnoses, in which their ISD diagnosis was changed to DM, with the median duration of misdiagnosis being 162 (IQR: 267) days. Among the overall cohort, CLE (4/5, 80.0%), unspecified dermatitis (11/17, 64.7%), and eczema (16/26, 61.5%) had the highest misdiagnosis rates. The ADM cohort (19/29, 65.5%) had a higher misdiagnosis rate compared to the myopathic DM cohort (17/44, 39%) (p = 0.04).
Among 36 misdiagnosed patients, 27 underwent skin biopsies. 24 showed interface dermatitis, while 3 demonstrated either perivascular or spongiotic dermatitis.
Conclusion: We highlight the prevalence of prolonged misdiagnosis and identify relevant dermatologic mimics in patients with DM. Misdiagnosis rate was notably higher in the ADM subtype, with eczema emerging as the most common dermatologic mimic. Skin biopsy was effective in correcting the misdiagnosed cases of DM. Robust clinicopathologic correlation is important for diagnosing cutaneous manifestations of DM.
To cite this abstract in AMA style:
Bao A, Tiniakou E, Christopher-Stine L, Mecoli C, Albayda J, Paik J, Kelly W, Kang J. Diagnostic Challenges of Dermatomyositis: A Retrospective Study of Its Dermatologic Mimics and Misdiagnoses [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/diagnostic-challenges-of-dermatomyositis-a-retrospective-study-of-its-dermatologic-mimics-and-misdiagnoses/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/diagnostic-challenges-of-dermatomyositis-a-retrospective-study-of-its-dermatologic-mimics-and-misdiagnoses/