Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Dermatoscopes are emerging as efficient, valuable alternatives to capillaroscopy for evaluating rheumatologic conditions. Second to systemic sclerosis, nailfold capillaroscopy abnormalities are most consistently reported in patients with dermatomyositis (DM) and less commonly reported in patients with systemic lupus erythematosus (SLE). Due to their heterogenous presentations and overlapping clinical features, it can be especially difficult to differentiate DM from SLE. We aimed to assess the potential use of evaluating nailfold changes with a dermatoscope as an additional diagnostic tool for distinguishing between DM and SLE.
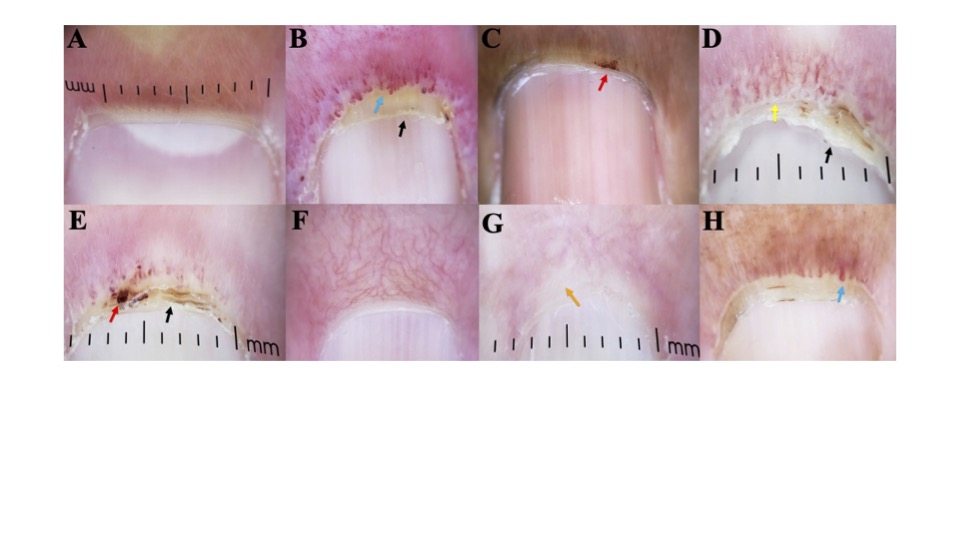
Methods: 53 DM patients, 22 with amyopathic DM, and 41 SLE patients with cutaneous LE (CLE) that met ACR/EULAR criteria for their respective diseases were included. Two images of each digit were taken using a DermLite DL4 dermatoscope attached to a smartphone adaptor. Images were assessed for presence of loop dilation, capillary dropout, capillary hemorrhage, visible subpapillary plexus, and cuticular dystrophy or overgrowth. Analysis was performed with a student’s t test.
Results: 96.2% of DM patients had nailfold changes in at least one digit compared to 65.9% of SLE patients (p< 0.001). In both conditions, nailfold changes were most often observed in the right fourth digit (94.3% DM, 48.8% SLE). 47.2% of DM patients had nailfold changes on all 10 digits compared to 9.8% SLE patients (p< 0.001). Moreover, DM patients had significantly higher frequencies of both loop dilation (81.1% vs. 31.7%, p< 0.001) and capillary dropout (67.9% vs. 24.4%, p< 0.001) compared to SLE patients. Capillary hemorrhages were also significantly more common in DM patients compared to SLE patients (60.4% vs. 29.3%, p=0.003). In addition to capillary changes, DM patients also exhibited significantly higher rates of cuticular overgrowth (66% vs. 39%, p< 0.009) and cuticular dystrophy (69.8% vs. 26.8%, p< 0.001) compared to SLE patients. Interestingly, the rates of visible subpapillary plexuses were similar between DM and SLE patients (21.9% vs. 30.2%, p=0.37).
Conclusion: Our study demonstrates that nailfold changes are significantly more prevalent and pronounced in DM patients compared to SLE patients. The high incidence of nailfold abnormalities, particularly loop dilation, capillary dropout, capillary hemorrhages, and cuticular changes, highlights the potential of dermatoscopic evaluation as a valuable diagnostic tool in distinguishing between DM and SLE. These findings support the use of dermatoscopy in clinical practice to aid in the differentiation of these two conditions, thereby enhancing diagnostic accuracy and patient management. Further studies with larger and more diverse populations are warranted to validate these findings and to explore the underlying mechanisms contributing to the observed differences.
To cite this abstract in AMA style:
Stone C, Faden D, Xie L, Lopes Almeida Gomes L, Dan J, Ricco C, Eldaboush A, Werth V. Nailfold Dermoscopy: A Valuable Tool for Differentiating Dermatomyositis from Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/nailfold-dermoscopy-a-valuable-tool-for-differentiating-dermatomyositis-from-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/nailfold-dermoscopy-a-valuable-tool-for-differentiating-dermatomyositis-from-systemic-lupus-erythematosus/