Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
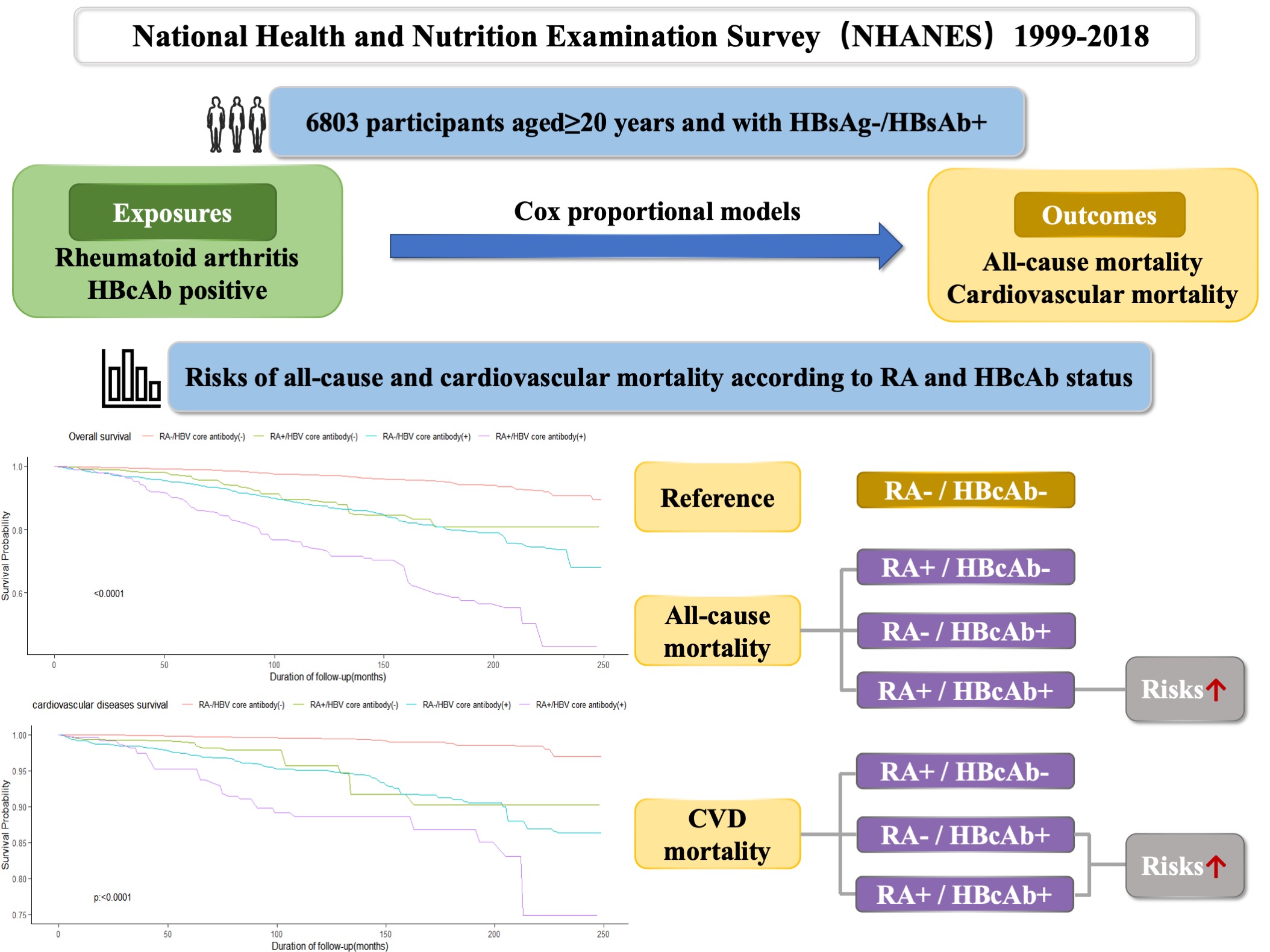
Background/Purpose: Rheumatoid arthritis (RA) and hepatitis B both have a high incidence and significant health impacts, possibly sharing a pathogenic connection. Notably, a considerable proportion of patients with RA test positive for hepatitis B core antibody (HBcAb), putting them at risk of HBV reactivation. This study is the first to explore the additive impacts of RA and HBcAb positive on all-cause and cardiovascular mortality in a population-based longitudinal study.
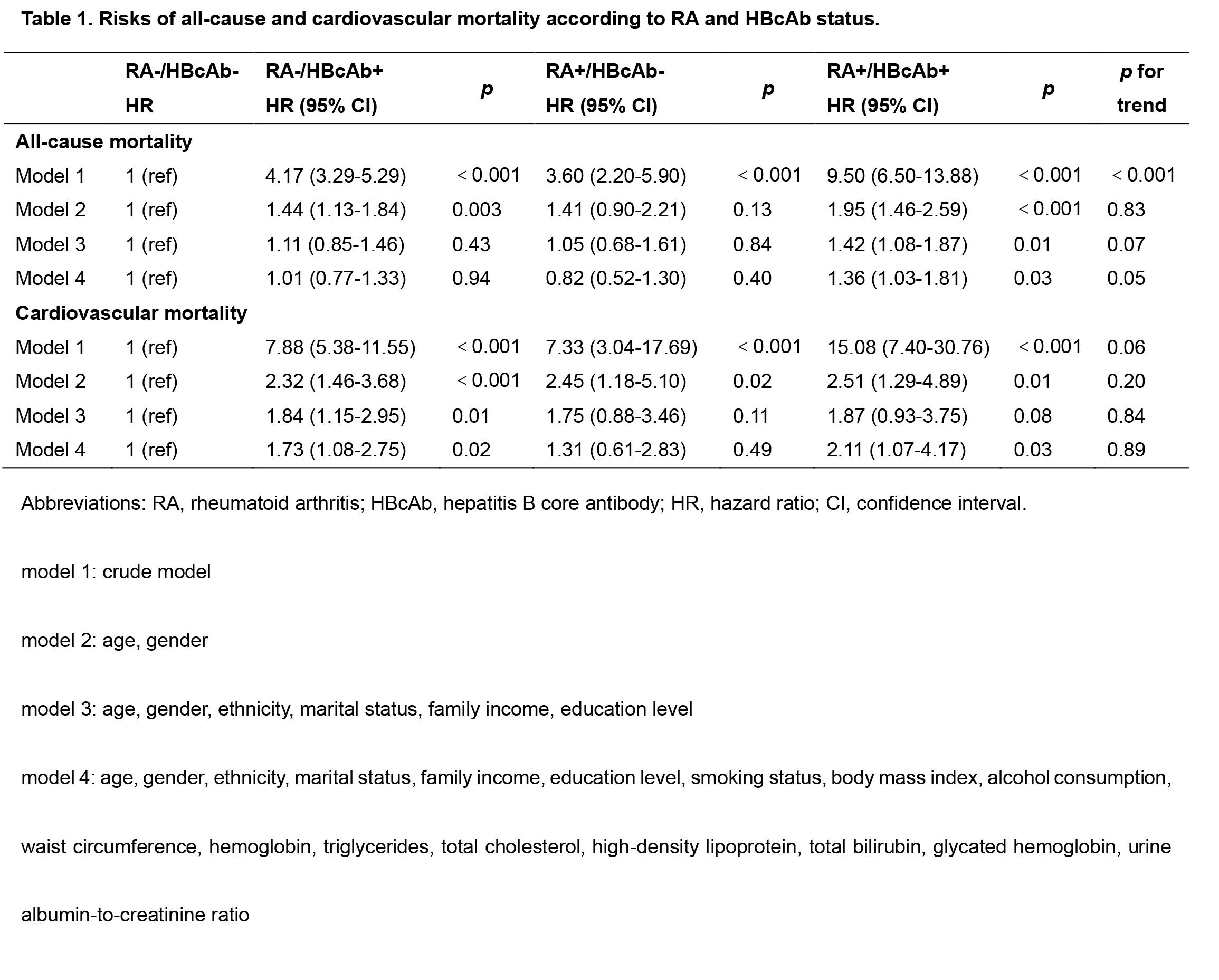
Methods: We analyzed data from the National Health and Nutrition Examination Survey (NHANES) spanning 1999 to 2018. Mortality data were obtained from National Death Index (NDI) records until December 31, 2019. Participants negative for hepatitis B surface antigen (HBsAg) and positive for hepatitis B surface antibody (HBsAb) were divided into four groups based on RA and HBcAb status. Utilizing Cox regression models adjusted for demographic and clinical variables, we explored the additive impact of RA and HBcAb on all-cause and cardiovascular mortality, with sensitivity analyses to ensure robustness.
Results: Among the 6803 HBsAg-/HBsAb+ participants, 4670 (68.6%) had neither RA or HBcAb (RA-/HBcAb-), 159 (2.3%) had RA but not HBcAb (RA+/HBcAb-), 1805 (26.5%) had HBcAb but not RA (RA-/HBcAb+), and 169 (2.5%) had both RA and HBcAb (RA+/HBcAb+). Compared to the RA-/HBcAb- group, the RA+/HBcAb+ group exhibited a higher risk of all-cause mortality (hazard ratio (HR)=1.36, 95% confidence interval (CI): 1.03-1.81, p=0.03), while the RA-/HBcAb+ (HR=1.01, 95% CI: 0.77-1.33, p=0.94) and RA+/HBcAb- (HR=0.82, 95% CI: 0.52-1.30, p=0.40) groups did not. For cardiovascular mortality, increased risks were observed in the RA-/HBcAb+ group (HR=1.73, 95% CI: 1.08-2.75, p=0.02) and the RA+/HBcAb+ group (HR=2.11, 95% CI: 1.07-4.17, p=0.03). In contrast, the RA+/HBcAb- group (HR=1.31, 95% CI: 0.61-2.83, p=0.49) did not show a significant risk increase. Among individuals with RA, those with both RA and HBcAb also had higher all-cause mortality (HR=1.66, 95% CI: 1.08-2.55, p=0.02) compared to those without HBcAb.
Conclusion: The coexistence of RA and HBcAb+ significantly increased the risk of both all-cause and cardiovascular mortality. Effective monitoring and management of these conditions are crucial to prevent either condition from worsening, which can subsequently lower mortality rates.
To cite this abstract in AMA style:
Yang L, Chen B, Xie Q, Yin G. Additive Impact of Rheumatoid Arthritis and HBcAb+ on All-cause and Cardiovascular Mortality [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/additive-impact-of-rheumatoid-arthritis-and-hbcab-on-all-cause-and-cardiovascular-mortality/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/additive-impact-of-rheumatoid-arthritis-and-hbcab-on-all-cause-and-cardiovascular-mortality/