Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Kawasaki Disease (KD), an acute pediatric vasculitis, requires inpatient management to prevent coronary artery disease. The Hospital for Sick Children (SickKids) sees about 100 cases of KD annually. Hospitalization and lack of reliable educational resources negatively impact the patient and family experience. By eliminating inefficiencies, reducing length of stay (LOS) and improving patient education, we aim to optimize patient experience and conserve healthcare resources. The objective is to optimize inpatient care for uncomplicated KD by reducing LOS by 33% at SickKids by April 2024.
Methods: This is a quality improvement time series using the Model for Improvement Framework. The project includes patients diagnosed and treated at SickKids. Stakeholders include Paediatric Medicine, Rheumatology, KD clinic, Transfusion Medicine and parent representatives.
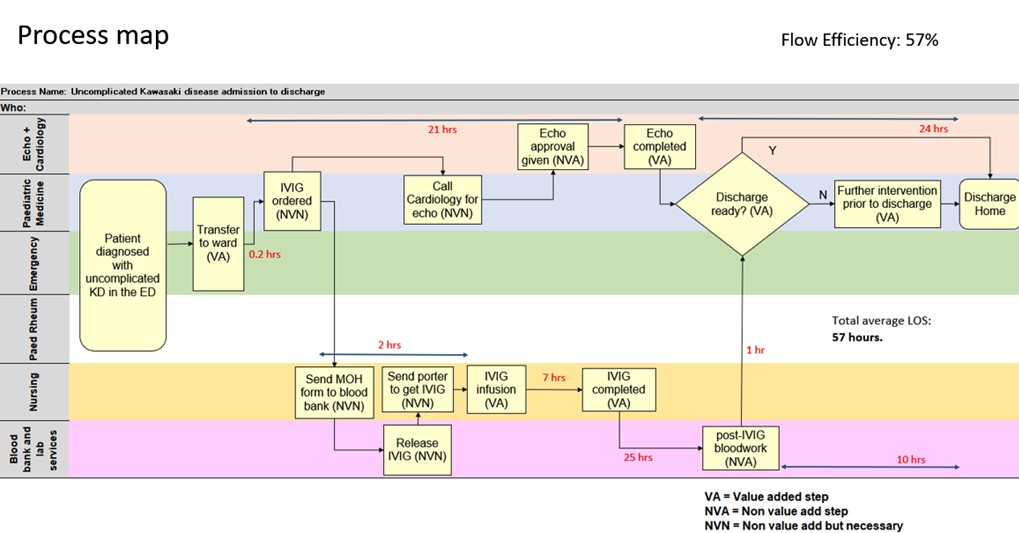
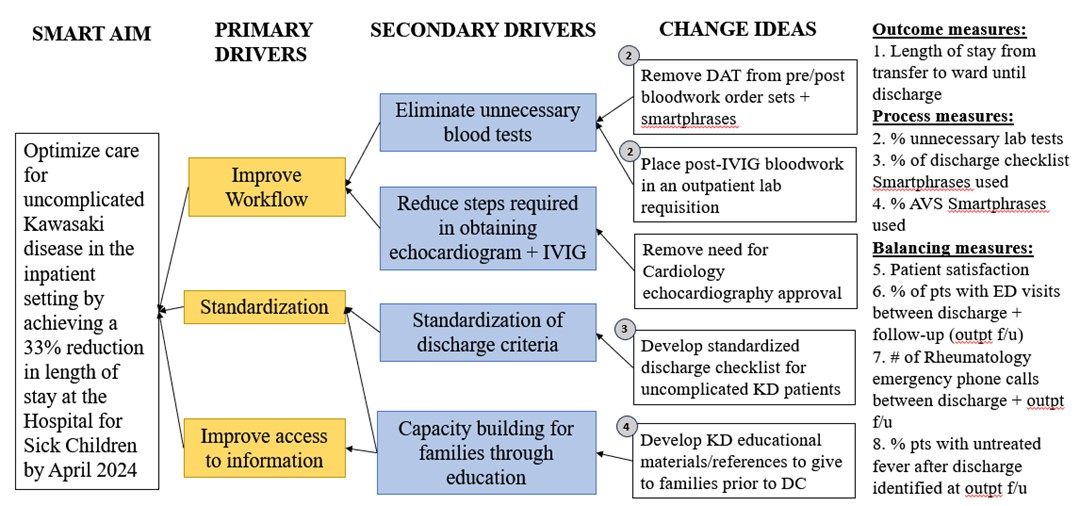
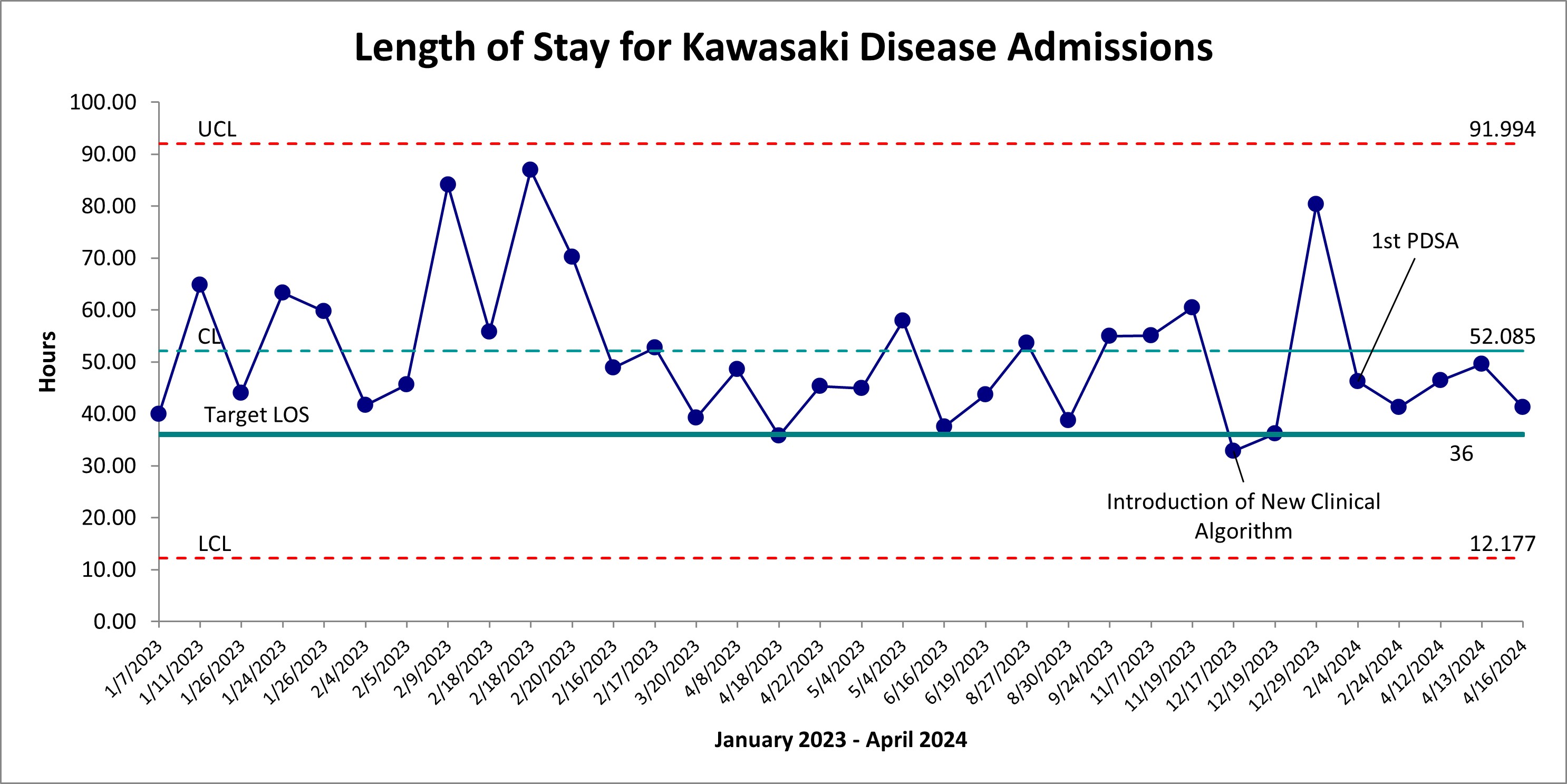
Chart review of patients with KD in 2023 demonstrated a baseline average LOS of 56 hours. Root cause analysis included focus groups, interviews, a process map outlining the KD admission (Fig. 1) and a Pareto diagram. A new clinical KD pathway was created incorporating 4 key change ideas: simplification of the echocardiography process, reduction of unnecessary blood tests, implementation of a discharge checklist and improvement of patient educational resources. Change ideas were linked to primary and secondary drivers of change through a driver diagram (Fig. 2).
The outcome measure is LOS for uncomplicated KD, which excludes those with refractory disease, concurrent complicated infection, shock and coronary artery dilation/aneursym on the hospital echocardiogram. Process and balancing measures included all patients admitted for KD. Process measures examined the fidelity of the change ideas. Balancing measures included rate of re-presentation to emergency care, untreated fever and patient satisfaction. Cost savings were estimated by calculating reductions in hours of admission as well as unnecessary bloodwork.
Results: Fifteen patients were admitted with KD since implementation of change ideas in December 2023, 8 had uncomplicated KD. The average LOS for uncomplicated KD was 41 hours, which is about a 25% reduction from baseline (Fig. 3). Process measures among 15 patients showed good uptake in change ideas. There was no increase in emergency services use among discharged patients, nor incidences of untreated fever. Six patients responded to the satisfaction survey with 100% feeling satisfied with the education received in hospital. There was an estimated $8936.75 in cost savings over 15 admissions.
Conclusion: The LOS for uncomplicated KD was reduced by 25% through strong uptake of the new simplified clinical KD pathway which did not negatively impact patient safety nor satisfaction. The project was strengthened by strong stakeholder relationships, patient/caregiver involvement and the use of automation and forced functions.
To cite this abstract in AMA style:
Chen A, Gamulka B, Palomer M, Yeung R. Optimizing Inpatient Kawasaki Disease Care [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/optimizing-inpatient-kawasaki-disease-care/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/optimizing-inpatient-kawasaki-disease-care/