Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Patients with autoimmune rheumatic diseases (RDs) have a high prevalence of oral manifestations and/or oral side effects from immunomodulatory medications. These factors combined with challenges impacting oral self-care can adversely impact oral health. We used qualitative methods to explore how patients with RDs perceive their oral health, to describe how patients and their health care providers (HCPs) approach oral care (self-care and professional dental care) and related any challenges/solutions related to this oral care, and to determine preferences for delivering oral health knowledge to patients and HCPs.
Methods: Semi-structured interviews were conducted virtually via Zoom with adult patients diagnosed with RD and pediatric and adult HCPs. Interview guides were informed by a patient living with RD. Interviews were recorded and transcribed verbatim, then independently reviewed by two analysts using thematic analysis based on a grounded theory approach. Each analyst read the transcripts multiple times, first to examine surface meaning and second to identify latent meaning, at which point initial codes were developed. Thereafter, the analysts discussed the codes and subsequently drafted, refined, and finalized the themes. Emerging themes are reported with supporting quotations.
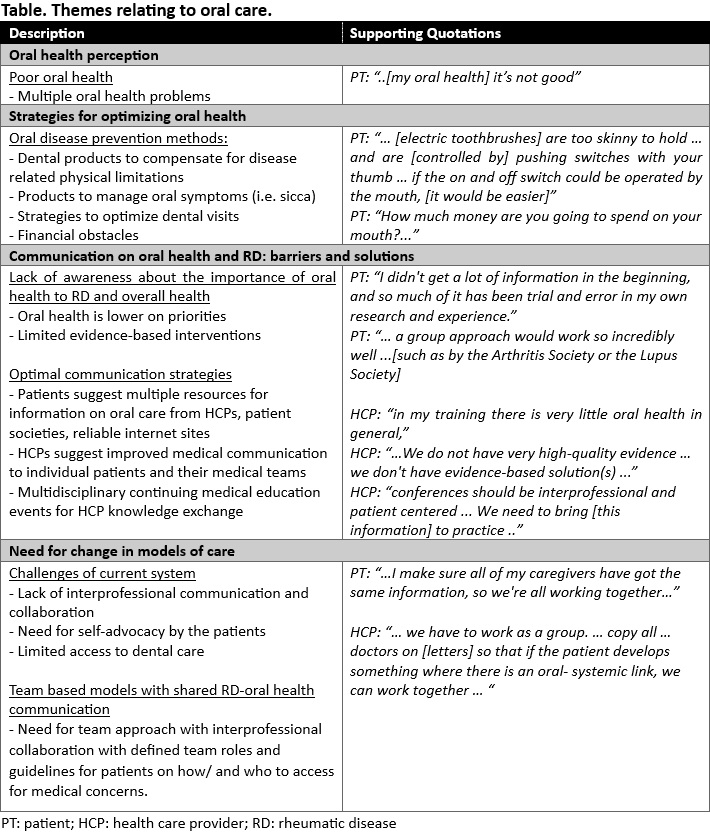
Results: Theme saturation was achieved after interviewing 9 patients (all female, age range 57-73 years) (rheumatoid arthritis n=3, juvenile idiopathic arthritis n=1, systemic lupus erythematosus n=2 systemic sclerosis n=1) and 3 HCPs (1 adult rheumatologist, 1 pediatric rheumatologist, 1 oral medicine and oral pathology dental specialist). On average interviews were 23 minutes long (range 10-40 minutes). All patients reported ≥1 oral health problem and 4 (55%) reported challenges with professional dental care. Gingival bleeding or recession, dry mouth, multiple tooth fractures, caries, fillings or crowns, oral ulcers and temporomandibular joint issues were the most frequently reported oral issues. We identified 4 themes relating to oral care: 1) Oral health perception and challenges 2) Strategies for optimizing oral health (including devises and products to overcome physical limitations and address oral symptoms), 3) Communication on oral health and RD: barriers and solutions (including need for education, evidence based strategies, and group learning activities), 4) Need for change in models of care (including multidisciplinary care and improved access to dental care) (Table).
Conclusion: Patients with RDs perceived substantial challenges with their oral health and professional dental care. Multiple dental products and creative strategies were utilized by the patients to overcome these challenges. Current educational resources were described as limited and unreliable. A multi-pronged communication strategy was suggested by the patients. An inter-professional team with holistic approach was proposed by patients and HCPs to help establish trusting relationships and more effective care.
To cite this abstract in AMA style:
Stavropoulou C, Billedeau C, Protudjer J, Hitchon C. A Qualitative Exploration of Oral Healthcare Needs Amongst Canadian Patients with Rheumatic Diseases and Their Providers [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/a-qualitative-exploration-of-oral-healthcare-needs-amongst-canadian-patients-with-rheumatic-diseases-and-their-providers/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-qualitative-exploration-of-oral-healthcare-needs-amongst-canadian-patients-with-rheumatic-diseases-and-their-providers/