Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Underserved communities in the USA face significant healthcare disparities, leading to poorer clinical outcomes and higher rates of chronic diseases. Socioeconomic barriers such as inadequate insurance coverage, poor health literacy, poverty, and cultural or linguistic differences impede patients’ access to care and exacerbate these health inequities. Patient navigator programs, like the Pharmaceuticals-sponsored initiative at SUNY Downstate Health Sciences University and Kings County Hospital (KCH), help guide individuals through a complex healthcare system and ensure patients receive timely and appropriate help.
Methods: The rheumatology and dermatology specialties established a two-site, dual-departmental patient navigator program at Downstate Medical Center and KCH in June 2021 and August 2022, respectively. The program recruited 153 patients from Arthritis clinics and 25 from dermatology clinics, identifying those with severe disease manifestations, poor adherence to appointments or medications, and/or language difficulties. Patients were randomly assigned to patient navigators, who were second-year medical students from SUNY Downstate Medical School. These students underwent standardized training, shadowed in rheumatology or dermatology clinics, and received structured didactics. Data on patient demographics, use of the patient navigator program, and communication methods were collected and stored in a HIPAA-compliant REDCap database.
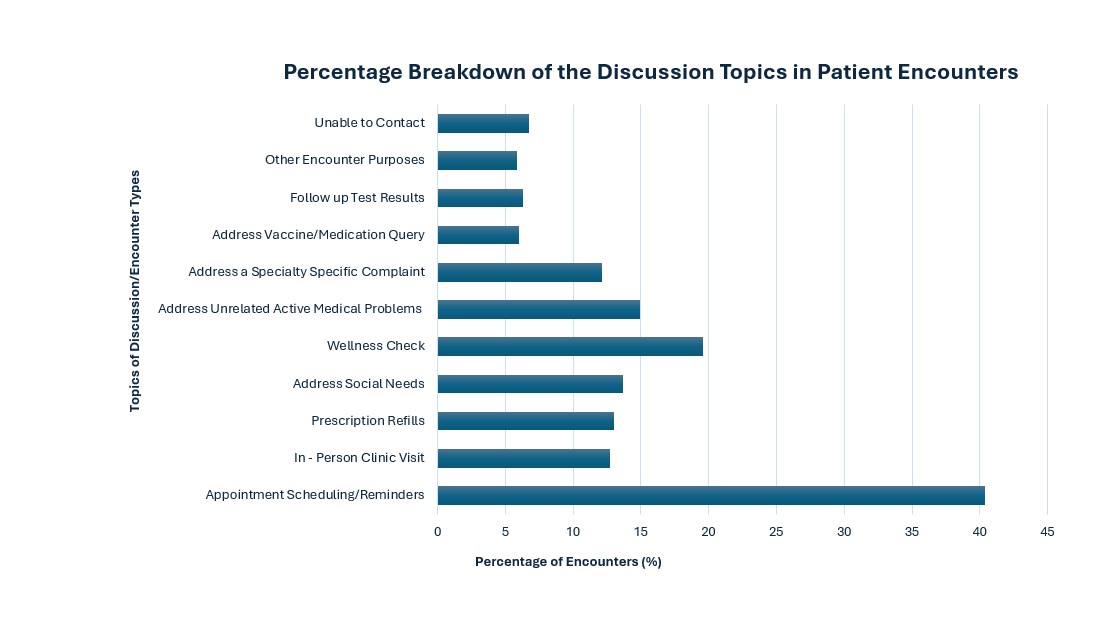
Results: The program enrolled 178 patients in rheumatology and dermatology, paired with 30 active patient navigators, resulting in a navigator-to-patient ratio of 1:5.93. The mean age of the patients was 48.5 years (SD 18.8). The male-to-female patient ratio was 1:5.13. The most common rheumatological and dermatological conditions among the enrolled patients were lupus (53.6%) and hidradenitis suppurativa (52.0%), respectively. Since the program’s initiation, there have been 716 encounters between patients and their navigators, with a median of 4.00 encounters per patient and a mean of 5.44 (SD 4.98). The primary communication method was by telephone, for 54.9% of encounters (393/716), followed by text (32.1%, 230/716). Navigators attended 91 clinic visits in person with their patients. Most encounters focused on appointment scheduling or reminders (40.3%), followed by wellness checks (19.6%), and addressing patients’ active medical issues unrelated to either specialty (14.9%). The mean number of issues addressed per encounter was 1.45 (SD 0.849). Multiple logistic regression analysis confirmed that patients were less likely to perceive wellness checks as helpful encounters, OR = 0.318 (95% CI: 0.114 – 0.760).
Conclusion: Addressing healthcare disparities in underserved communities can improve health outcomes and achieve equity. Patient navigator programs implemented at SUNY Downstate and KCH play a vital role in bridging gaps in care and providing continuity and essential support for high-risk patients. Further research will compare patients’ clinic attendance rates before and after patient navigator assignment.
To cite this abstract in AMA style:
Kurup M, Shadid G, Pak J, Moncayo A, Kabani N, Kabir S, Glick S, Ginzler E. Improving Healthcare Access in Underserved Brooklyn Communities: A Comprehensive Multispecialty Patient Navigator Program [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/improving-healthcare-access-in-underserved-brooklyn-communities-a-comprehensive-multispecialty-patient-navigator-program/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/improving-healthcare-access-in-underserved-brooklyn-communities-a-comprehensive-multispecialty-patient-navigator-program/