Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: People with rheumatoid arthritis (RA) are at an increased risk of heart failure (HF), which is among the most burdensome chronic conditions and a leading cause of hospitalization in the U.S. A characteristic feature of severe HF is recurrent exacerbations that often lead to hospitalization. HF risk in RA has been evaluated exclusively using traditional time-to-event analyses, which evaluate an initial HF event and do not account for repeated hospitalizations. As such, we aimed to examine the risk of HF in RA using recurrent event analysis approaches.
Methods: We constructed a retrospective, matched cohort of RA patients matched up to 10 comparators on age, sex, and VA enrollment year between 2000 and 2019. Patients with prevalent HF were excluded, and the remaining cohort was followed to death or end of study period (1/2020). Incident and subsequent HF events were identified as a primary hospital discharge diagnosis (VA and linked Medicare data) or HF-related death (National Death Index). A HF hospitalization was considered recurrent if it occurred ≥7 days following a prior hospital discharge date. Re-admissions occurring earlier were combined and modeled as one admission. Average length of stay and time between admissions were described. Three recurrent event analytic approaches were used. First, incidence rate ratios for HF events were calculated in RA vs. non-RA using Poisson regression (count method). Second, RA-related risk of recurrent HF was tested in Prentice, Williams, and Peterson Total Time (PWP-TT) models, a recurrent event survival analysis, which assumes a varying hazard between incident and subsequent events, stratifying the model at each event. Third, we used Anderson-Gill models, which assume a common baseline hazard for all events. Models were stratified on matched pairs and adjusted for demographics, smoking status, body mass index, comorbidity burden, and healthcare utilization.
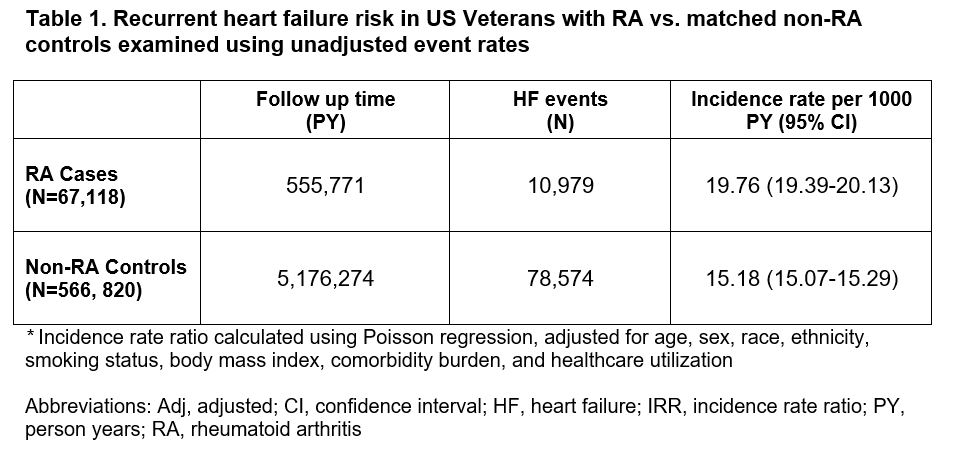
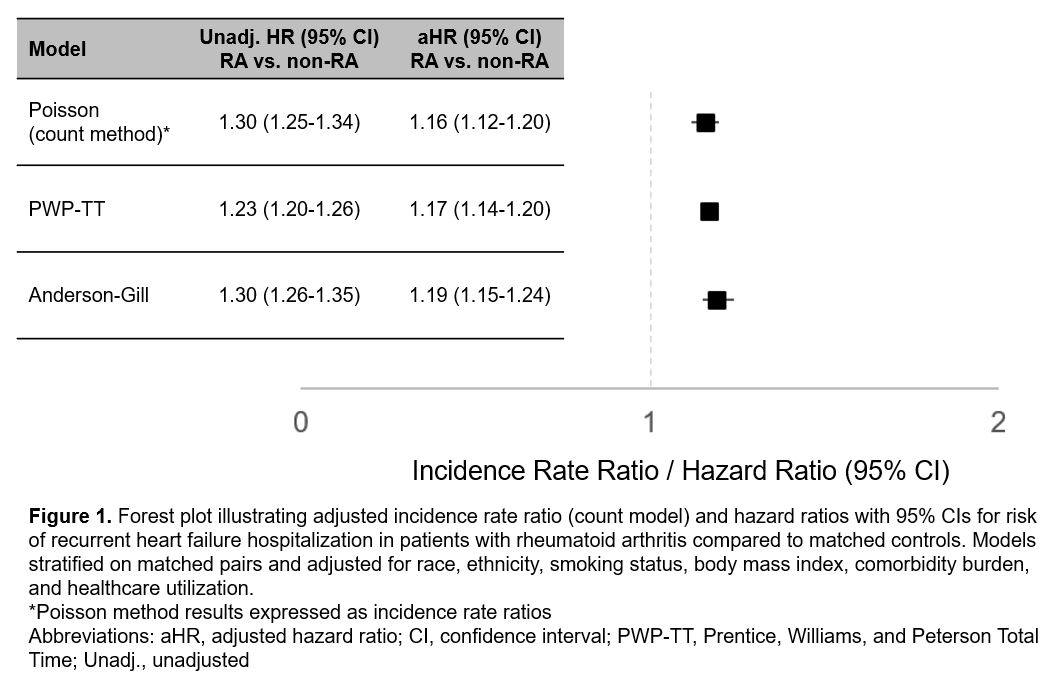
Results: We matched 67,118 RA patients (mean age 62 years, 87% male) to 566,820 patients without RA. Over 5,730,382 person-years of follow up, we identified 10,979 HF events in RA (19.8 events per 1000 PY) vs. 78,574 in non-RA (15.2 events per 1000 PY; Table 1). The average length of HF-related hospital stay was similar between groups (mean 6.6 days in RA, 6.8 days in non-RA), while time between HF-related hospitalizations was shorter in RA (mean 316 days vs. 349 days, p< 0.001). The adjusted incidence rate ratio for HF events in RA vs. non-RA using the count method was 1.16 (95% CI 1.12-1.20; Figure 1). In recurrent event survival analyses, RA patients were at similarly increased risk of recurrent HF events when analyzed using PWP-TT (aHR 1.17 [1.14-1.20]; Figure 1) and Anderson-Gill (aHR 1.19 [1.15-1.24]) methods.
Conclusion: In this large, matched cohort study, people with RA were observed to be at a significantly increased risk of recurrent HF events using recurrent event analysis approaches. These findings further underscore the burden of HF in RA throughout the disease course and emphasize the importance of improving HF management to prevent recurrent HF events in this high-risk population.
To cite this abstract in AMA style:
Johnson T, Yang Y, Roul P, Baker J, Kunkel G, brian S, Cannon g, Mikuls T, England B. Recurrent Heart Failure Hospitalization in Rheumatoid Arthritis: A National Veterans Affairs Matched Cohort Study [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/recurrent-heart-failure-hospitalization-in-rheumatoid-arthritis-a-national-veterans-affairs-matched-cohort-study/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/recurrent-heart-failure-hospitalization-in-rheumatoid-arthritis-a-national-veterans-affairs-matched-cohort-study/