Session Information
Date: Sunday, November 17, 2024
Title: Abstracts: RA – Diagnosis, Manifestations, & Outcomes III: Best Day (RA Subpopulations)
Session Type: Abstract Session
Session Time: 3:00PM-4:30PM
Background/Purpose: Fracture incidence rates (IRs) are higher in men and women with rheumatoid arthritis (RA) than those without RA, especially for those with higher RA disease activity. In persons with RA worldwide, the IR per 1,000 person-years (PYs) of any fragility fracture is 15.3 (95% confidence interval (CI): 10.4-22.5) and the IR of hip fracture is 4.3 (95% CI: 2.3-8.3), but IRs for modern U.S. cohorts have not been described. This study describes fracture IRs and incidence rate ratios (IRRs) in persons with RA in the U.S. by disease activity level.
Methods: We conducted a retrospective cohort study (2016-2018) using Rheumatology Informatics System for Effectiveness (RISE) data linked to Medicare claims. RISE is a national, electronic health record-enabled registry of participating rheumatology practices. We included men and women ≥ 65 years old with RA (≥ 2 visits with RA codes ≥ 30 days apart) and required continuous Medicare (Parts A, B) coverage in 2016 and January 2017. RA disease activity was ascertained from the most recent visit prior to 1/1/2017 where disease activity was documented, and categorized as remission, low, moderate, or high, regardless of measure used. Incident hip and major osteoporotic fracture (MOF: first of distal forearm, hip, humerus, or vertebral fracture) were determined using validated case qualifying Medicare claims-based fracture episode definitions. Participants were followed from 1/1/2017 until the first of: incident fracture (hip or MOF, respectively), death, gap in Medicare enrollment (Parts A, B, or D), or end of the study period (12/31/2018). IRs and 95% CIs for hip fracture and MOF overall and stratified by sex and disease activity level were reported. IRRs for disease activity level were estimated by dividing the IR of individuals at each disease activity level by the IR of those in remission, and 95% CIs computed.
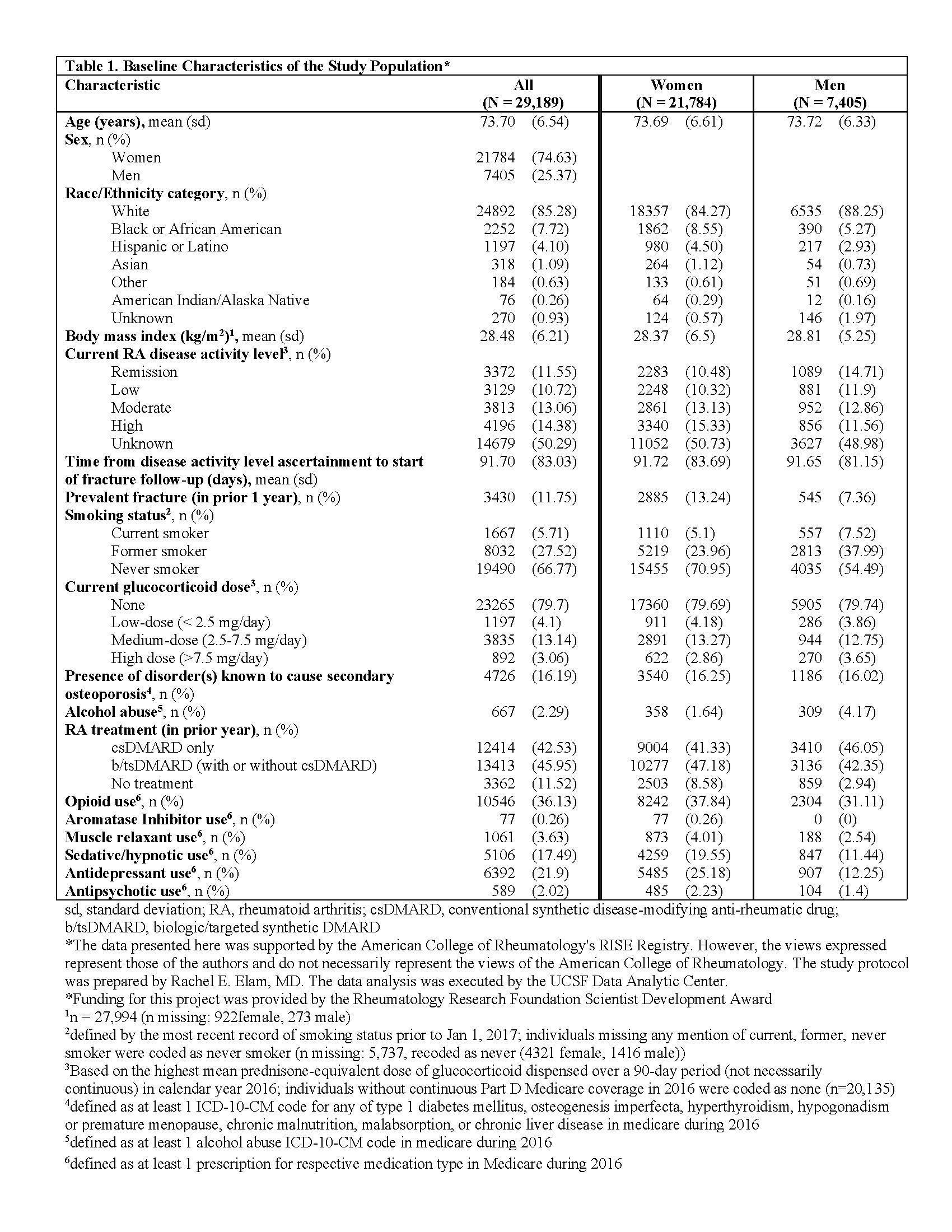
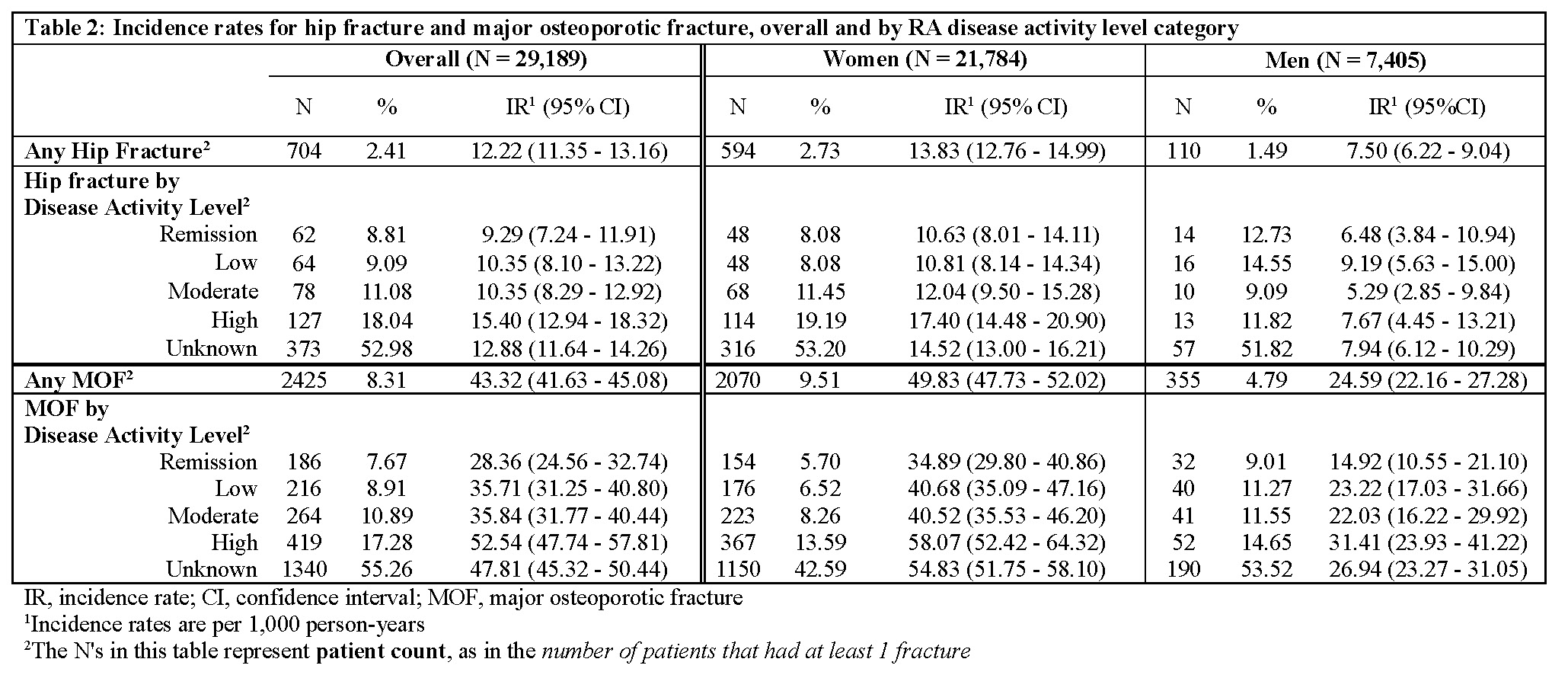
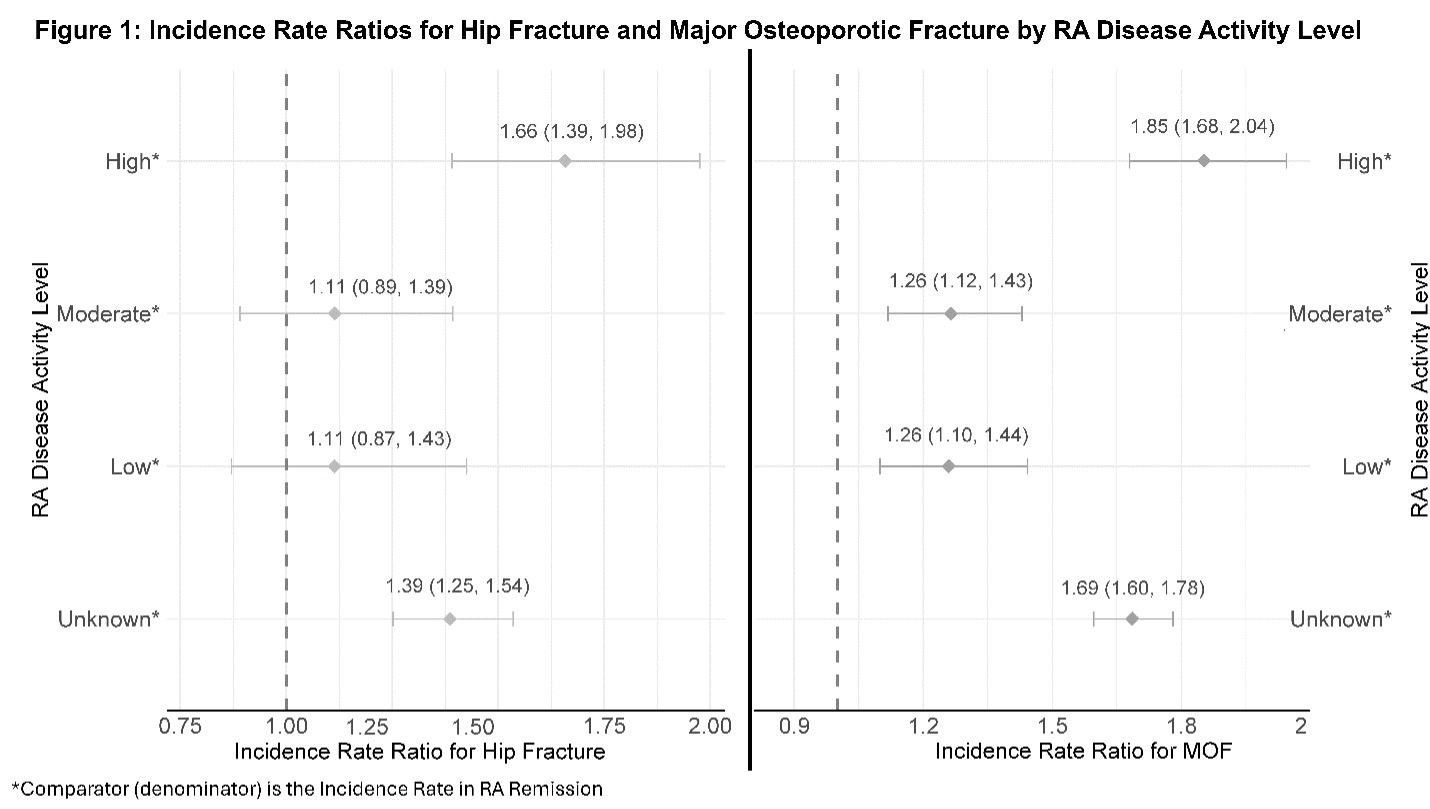
Results: Of 29,189 study participants (mean age: 73.7 years, 75% women, 85% White; Table 1), 704 persons (594 women) fractured a hip and 2,425 persons (2,070 women) had a MOF. The overall IR for hip fracture was 12.2 (95% CI: 11.4-13.2) per 1,000 PYs and for MOF was 43.3 (95% CI: 41.6-45.1). The IRs for hip and MOF increased with higher disease activity overall and in women, while in men, this increase was observed only for MOF (Table 2). High disease activity was associated with higher rates of hip fracture (Figure 1). Disease activity above remission was associated with higher rates of MOF (Figure 1).
Conclusion: In persons with RA aged 65 years and older, hip fracture and MOF are more common in patients with RA disease activity above remission, especially those with high disease activity. These findings emphasize the importance of bone health assessments in RA, particularly among those with high disease activity, as the risk of hip fracture and MOF are significantly increased in the following two years.
To cite this abstract in AMA style:
Elam R, Kersey E, Li J, Schmajuk G, Carbone L. Fracture Incidence Rates in Persons with Rheumatoid Arthritis by Disease Activity Level [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/fracture-incidence-rates-in-persons-with-rheumatoid-arthritis-by-disease-activity-level/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/fracture-incidence-rates-in-persons-with-rheumatoid-arthritis-by-disease-activity-level/