Session Information
Session Type: Abstract Session
Session Time: 3:00PM-4:30PM
Background/Purpose: Inflammatory arthritis is one of the most common immune-related adverse events (irAEs) resulting from immune checkpoint inhibitors (ICIs). We hypothesized that T cells present in joints damaged by osteoarthritis (OA) are primed for ICI induced on-target off-tumor immune responses, resulting in increased irAE-arthritis risk in OA.
Methods: This case-control study evaluated the prevalence of OA in ICI treated patients who develop inflammatory irAE-arthritis (cases) vs. other irAEs (non-arthritis) vs. no irAEs (controls). We defined OA based on the ICD-10 codes and/or Kellgren and Lawrence radiographic criteria. Synovial and peripheral blood mononuclear cells were analyzed using a multiparameter spectral flow panel, followed by unsupervised clustering, UMAP dimensionality reduction and enrichment analysis.
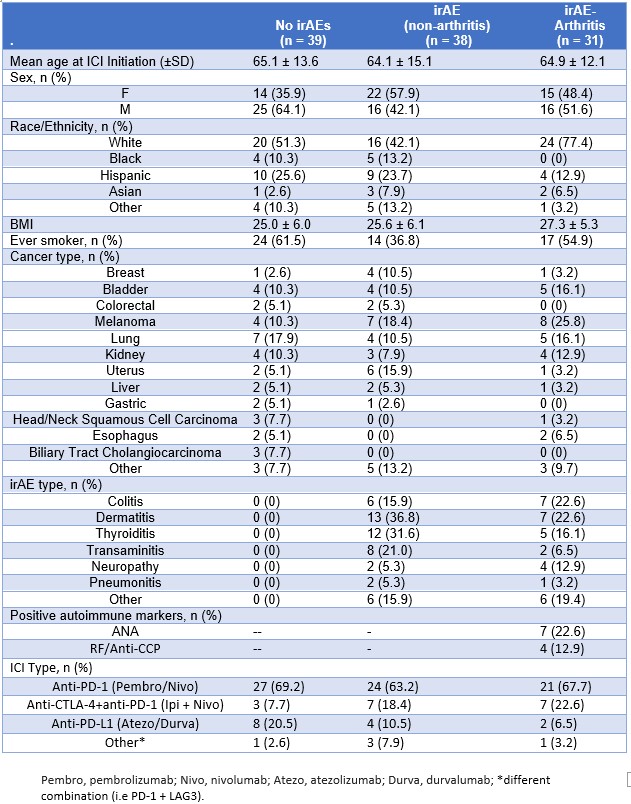
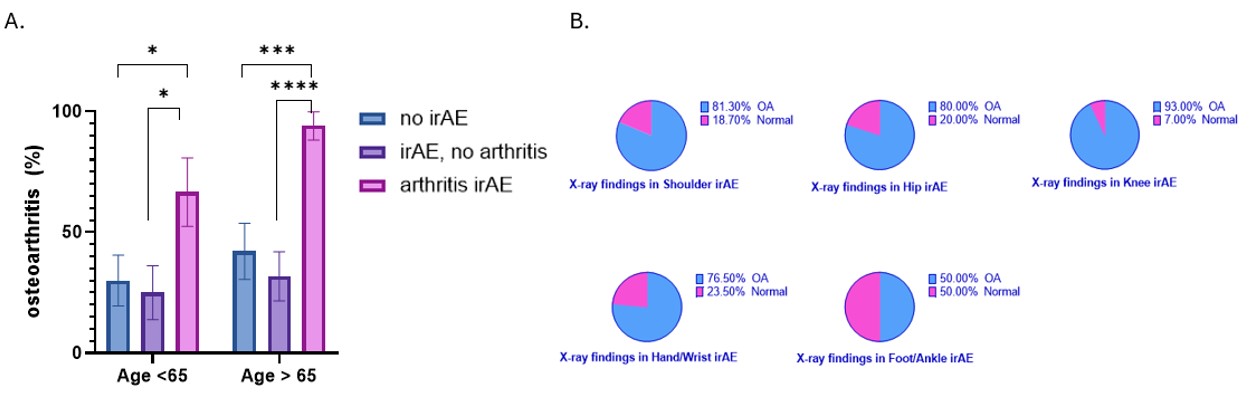
Results: 108 patients who received ICI treatment were included in the study: 31 with irAE-arthritis, 38 with non-arthritis irAE, and 39 with no irAEs. Patient characteristics are summarized in Table 1. The prevalence of OA was increased in the irAE-arthritis group (83.9%) as compared to 28.9% (p< 0.001) in non-arthritis irAEs and 35.9% (p< 0.001) in the no irAEs groups, Fig.1A. In multivariable analyses, irAE-arthritis was independently associated with the presence of OA (OR 75.5, 95% CI 6.3-685.5), history of smoking (OR 16.5, 95% CI2.0-137.6) and BMI (OR 1.2, 95% CI 1.1-1.4) when controlling for age, gender and race. The prevalence of OA in the irAE-arthritis-affected joints is shown in Fig 1B.
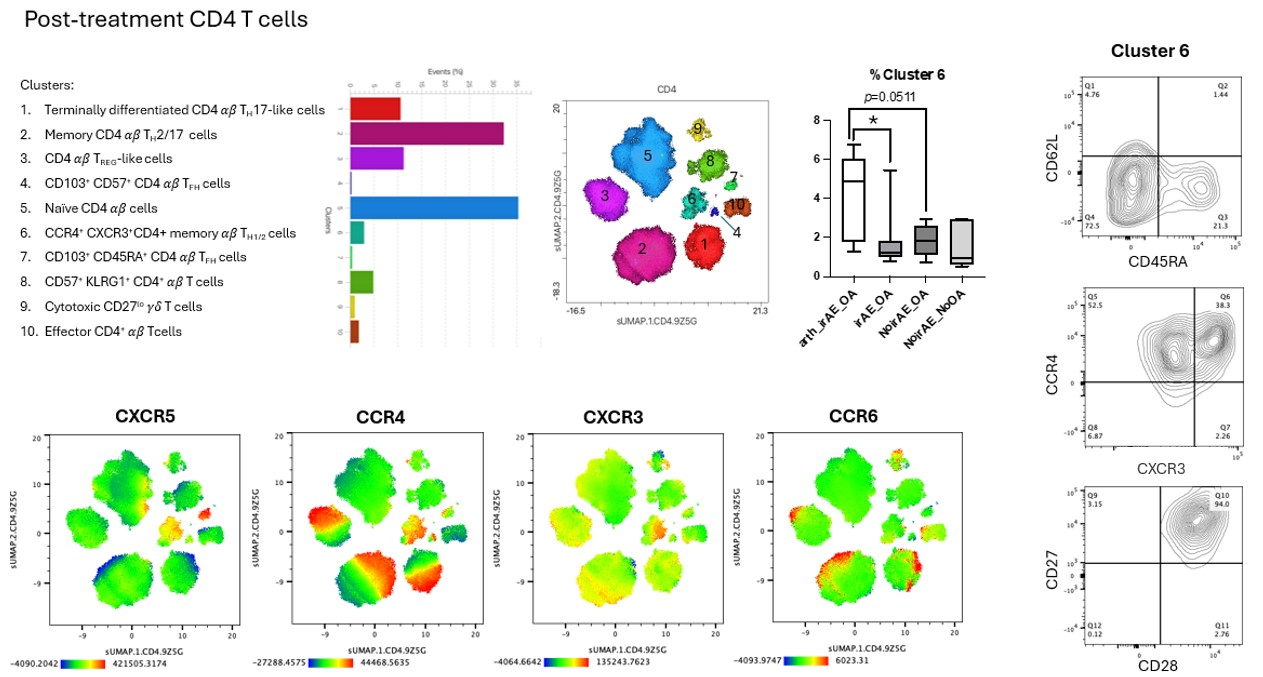
Analysis of OA synovial fluid (ICI untreated) identified the presence of CD8+ and CD4+ αβ T lymphocytes (58.55±61.50 cells/uL) which highly express PD-1. Of these, 30% had the phenotype of resident memory T cells (CD69+ CD103+). Following ICI treatment, analysis of PBMCs from OA patients revealed an expanded CD4+ T cell cluster 6 in irAE-arthritis as compared to non-arthritis irAE (p< 0.05) or no irAEs (p=0.05), Fig 2. Further analysis identified this cluster as an unusual memory CD4+ T cell subset expressing CCR4 and CXCR3, but lacking CCR6 and CD161. Additionally, we found expanded CD8+ TEMRA cells in irAE-arthritis vs. non-arthritis irAE (p=0.02).
Conclusion: There is a significant association between irAE-arthritis and the prevalence of OA in the affected joints. Resident memory T cells present in the OA synovial fluid may contribute to the development of irAE-arthritis. Expanded CD8+ TEMRA and CD4+ memory CCR4+CXCR3+ T cell populations were found in OA patients who develop irAE arthritis compared to controls.
* These authors contributed equally to this work.
To cite this abstract in AMA style:
Portnoy D, Piola M, Hao L, Winchester R, Mor A, Gartshteyn Y. Osteoarthritis Is a Risk Factor for Inflammatory Arthritis in Cancer Patients Treated with Immune Checkpoint Inhibitors [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/osteoarthritis-is-a-risk-factor-for-inflammatory-arthritis-in-cancer-patients-treated-with-immune-checkpoint-inhibitors/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/osteoarthritis-is-a-risk-factor-for-inflammatory-arthritis-in-cancer-patients-treated-with-immune-checkpoint-inhibitors/