Session Information
Session Type: Abstract Session
Session Time: 1:00PM-2:30PM
Background/Purpose: Little is known of the factors that trigger disease relapses/flares in patients with rheumatoid arthritis (RA). The underpinning mechanisms have been difficult to study because of the unpredictable nature of flare. The BIOlogical Factors that Limit sustAined Remission in rhEumatoid arthritis (BIO-FLARE) study1 is an experimental medicine study of ‘synchronised’ RA flares. This is achieved by stopping treatment in RA patients in clinical remission receiving conventional synthetic (cs)DMARDs. Subsequently, approximately 50% flare within 6 months, the remainder maintaining drug-free remission (DFR). In the current analysis we have measured circulating proteins in sequential blood samples following treatment cessation.
Methods: Individuals with RA receiving methotrexate, sulfasalazine and hydroxychloroquine, singly or in combinations, in clinician-defined remission with a DAS28-CRP < 2.4 were recruited into BIO-FLARE. Treatment was stopped and participants monitored over 24 weeks, and serum stored at 0, 2, 5, 8, 12 and 24 weeks. Flare was defined as DAS28-CRP ≥3.2 at any study visit, or DAS28-CRP ≥2.4 on two occasions within a 14-day period. Soluble serum mediators were detected by the NULISAseq™ Inflammation Panel 250 (Alamar Biosciences)2. Following data normalisation and quality control, differential expression analysis was performed using the NULISAseqR package. An unadjusted significance threshold (p< 0.05) was used in the baseline analysis for discovery purposes, whereas a false discovery rate (FDR) adjusted p value < 0.05 was deemed significant in the longitudinal data.
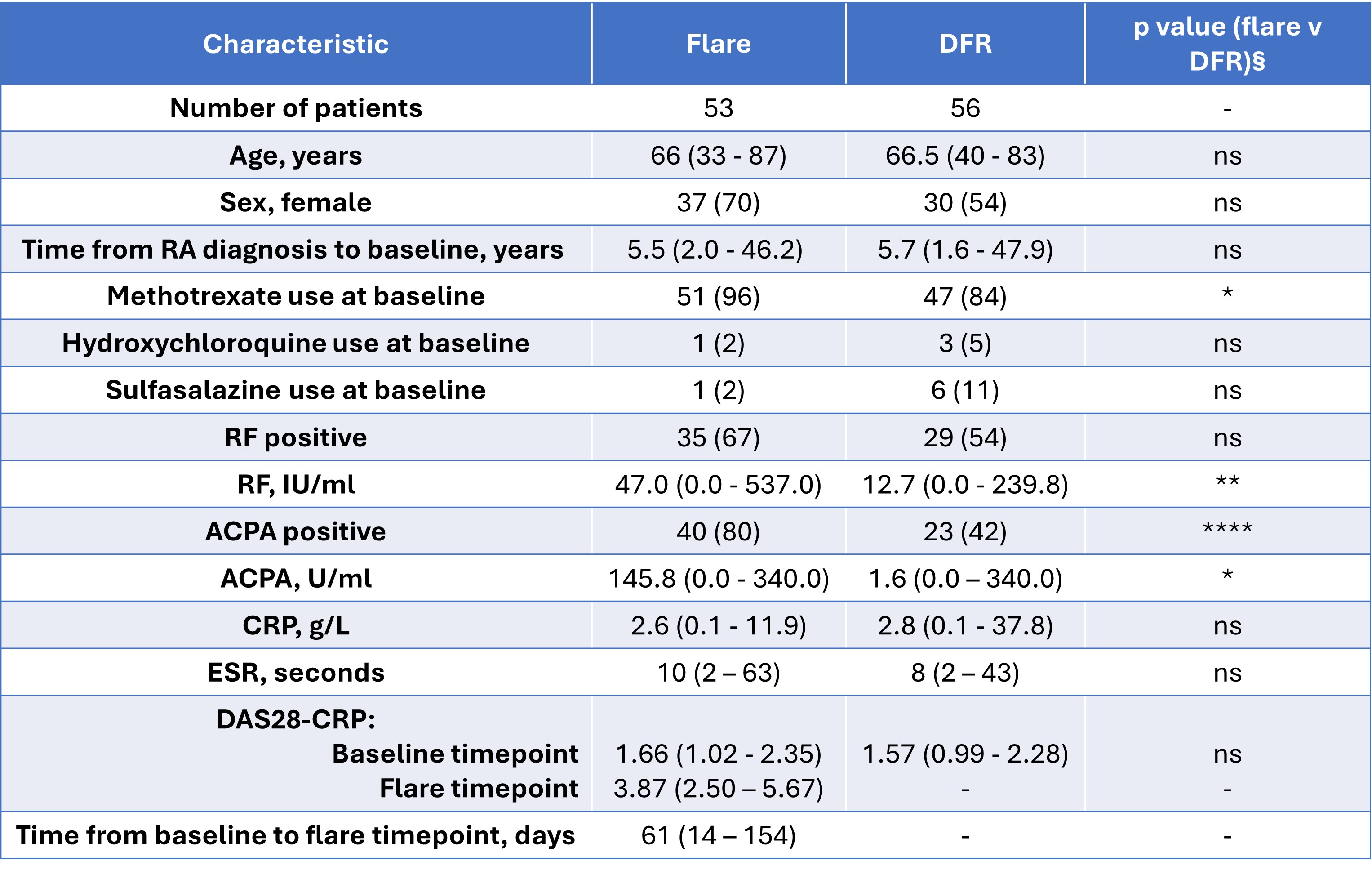
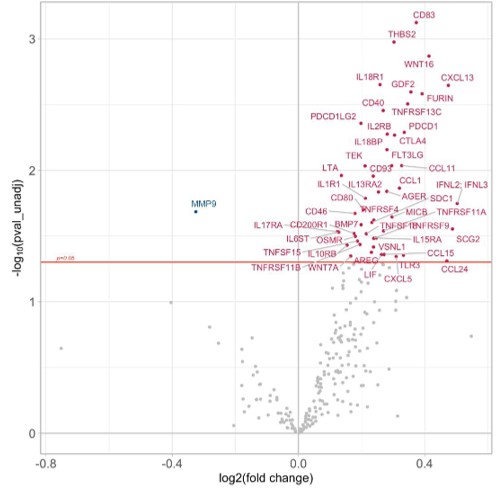
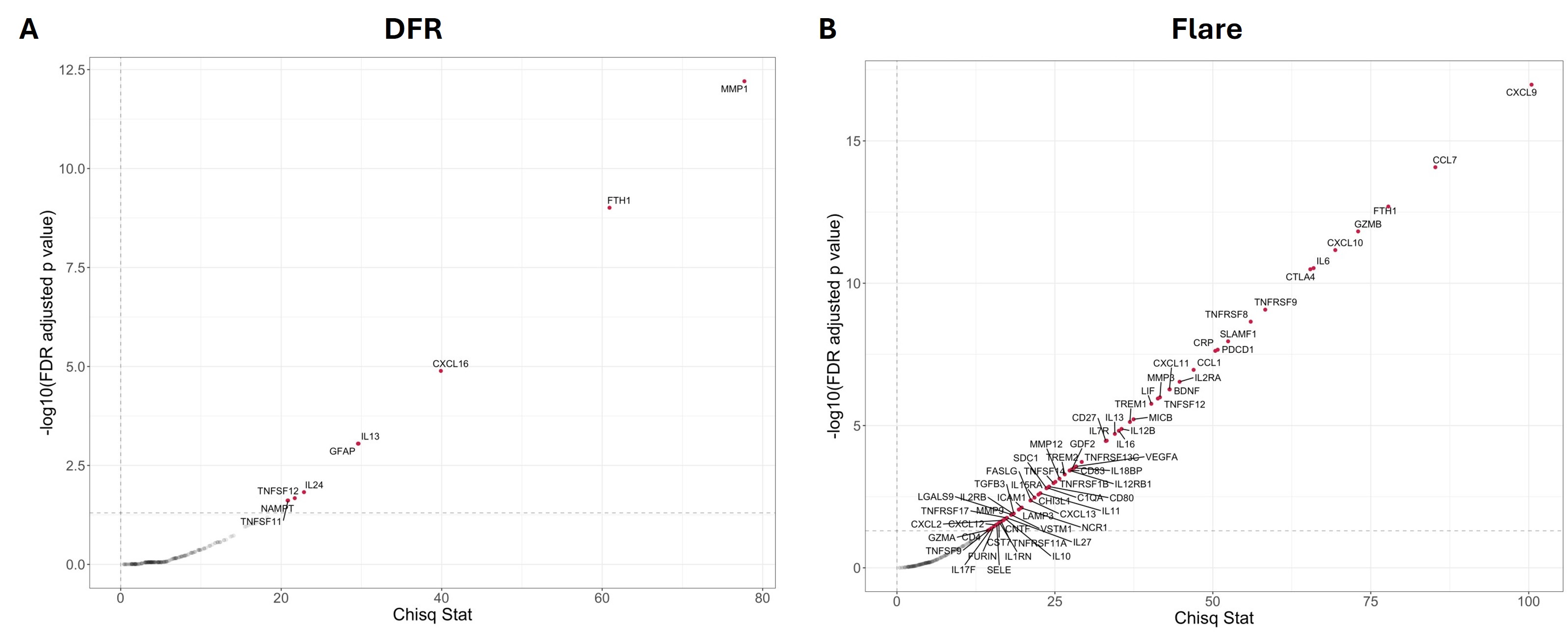
Results: At baseline, participants who subsequently flared and those who maintained DFR were well matched clinically, with the exception of RF/ACPA titres (Table 1). In contrast, NULISAseq analysis revealed differences in a number of inflammatory mediators, such as CXCL13 and soluble PD-1 (PDCD1), and immunoregulatory molecules, such as soluble CD83 and CTLA-4, all of which were elevated in the flare group at baseline (Figure 1). When assessing changes in soluble mediators across time from the point of DMARD withdrawal, few changes were detected in the DFR group (Figure 2A), whereas a number of inflammatory mediators, such as CXCL9, CXCL10, granzyme B and IL-6, increased in the flare group (Figure 2B).
Conclusion: Even prior to DMARD cessation, individuals who subsequently flare following csDMARD withdrawal display a unique soluble proteome, indicative of immune activation and regulation. Other mediators increase towards the point of flare, providing potential insights into flare physiology. Our ultimate goal is to develop biomarkers that will facilitate targeted treatment withdrawal in patients in remission, and to generate knowledge that may aid relapse prevention by appropriately targeted therapeutics.
References
- Rayner F et al. BMC Rheumatol. 2021
- Feng W et al. Nat Commun. 2023
To cite this abstract in AMA style:
Anderson A, Rayner F, Degnan A, Wilson I, Diboll J, Sim J, Melville A, Siebert S, McInnes I, Goodyear C, Hilkens C, Filer A, Raza K, Buckley C, Baker K, Pratt A, Isaacs J. Using Circulating Soluble Serum Mediator Profiles to Understand the Mechanisms Driving Disease Flare and Drug-free Remission in Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/using-circulating-soluble-serum-mediator-profiles-to-understand-the-mechanisms-driving-disease-flare-and-drug-free-remission-in-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/using-circulating-soluble-serum-mediator-profiles-to-understand-the-mechanisms-driving-disease-flare-and-drug-free-remission-in-rheumatoid-arthritis/