Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Mixed connective tissue disease (MCTD) is a rare systemic disorder that belongs to connective tissue diseases (CTD). Few studies are available on MCTD treatment. Taking advantage of the French MCTD cohort (1), we conducted an observational study to describe the therapeutic strategy used in MCTD.
Methods: We conducted an observational study within the French MCTD cohort (1). This cohort includes patients diagnosed with MCTD according to at least one of the four diagnostic criteria for MCTD and who, at disease onset, did not fulfill classification criteria for systemic sclerosis, systemic lupus erythematosus, Sjögren’s syndrome, idiopathic inflammatory myopathies, nor rheumatoid arthritis. Data regarding treatment were collected at MCTD diagnosis, during follow-up, and at the last follow-up (LFU).
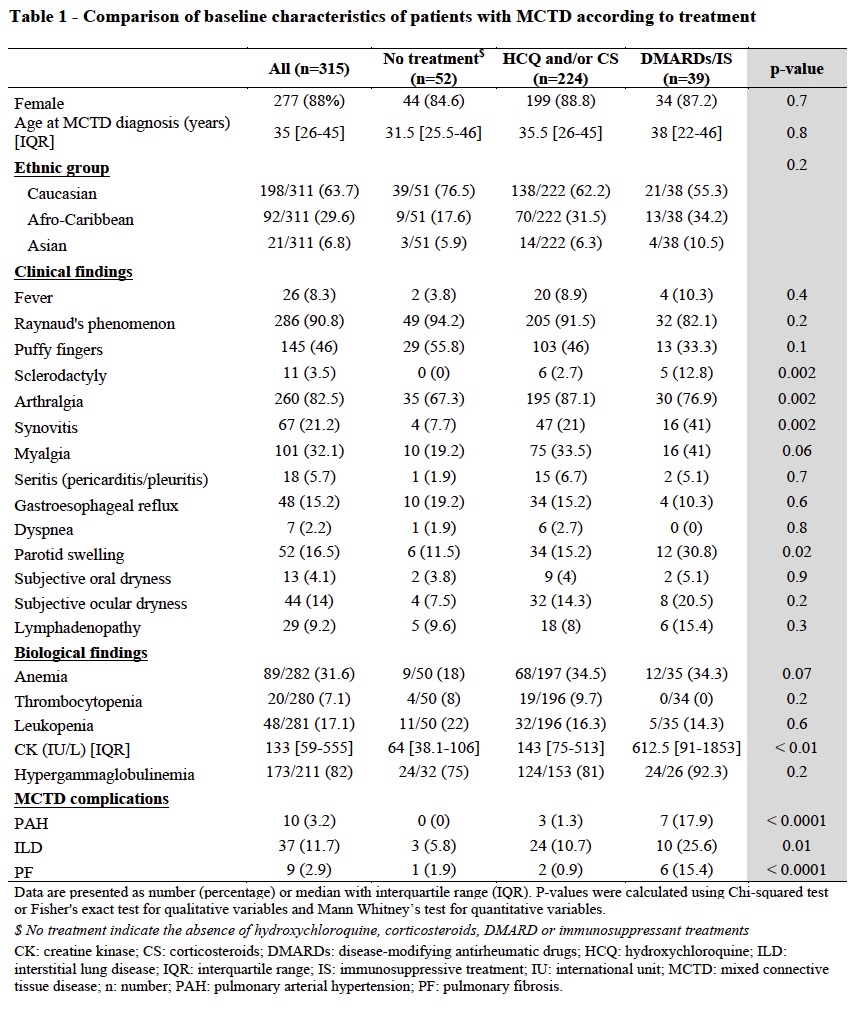
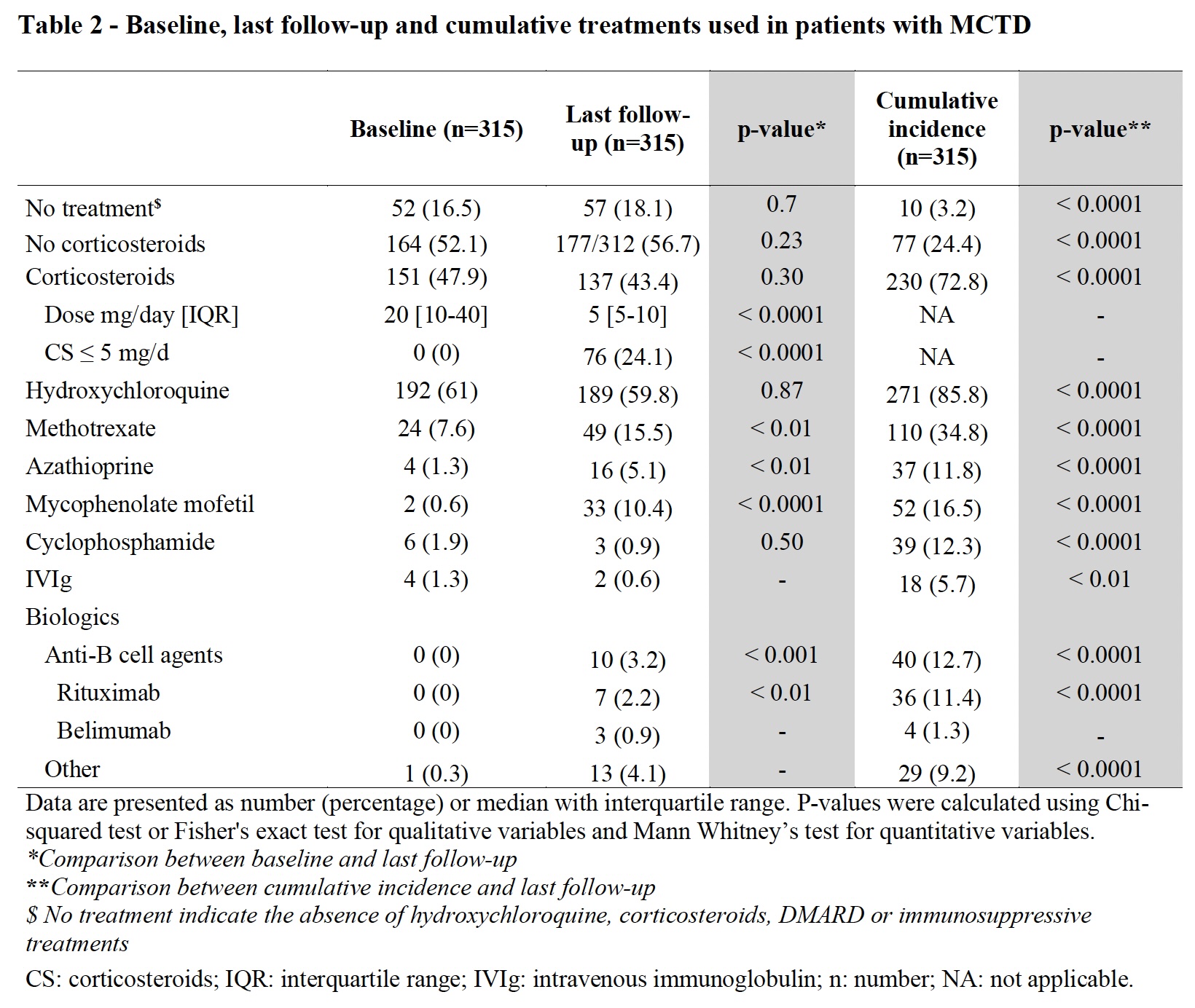
Results: Of the 330 MCTD patients enrolled in the French MCTD cohort, 315 (96%) were included and followed up during 96 [40-156] months. Patient’s main characteristics and treatments are described in Table 1 and Table 2. At disease onset, 52 (17%) patients were treated with calcium channel blockers and/or nonsteroidal anti-inflammatory drugs only and/or no treatment at all, while 36 (11%) were treated with corticosteroids (CS) alone, 188 (60%) with hydroxychloroquine (HCQ) without disease-modifying antirheumatic drugs (DMARDs) or immunosuppressive treatment (IS), and 39 (12%) with DMARDs and/or IS. At LFU, patients received a lower median dose of CS compared to baseline (5 [5-10] vs 20 [10-40] mg/day; p< 0.001) and more frequently received DMARDs and/or IS than at baseline (p< 0.001). Overall, 10 (3%) patients remained treatment-free, 77 (24%) CS-free, and 148 (47%) were only treated with HCQ and/or low-dose CS at LFU. Among IS, anti-B cell agents were used in 39 (12%) patients during follow-up.
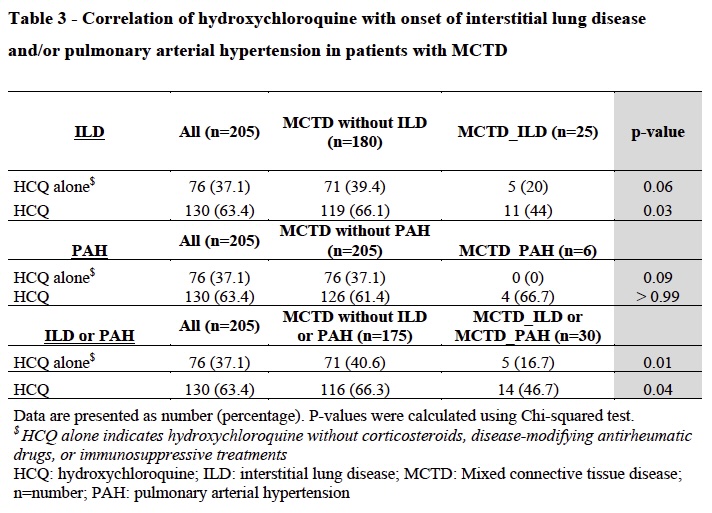
At baseline, patients with sclerodactyly (p=0.002), synovitis (p=0.002), dyspnea (p=0.02), pulmonary arterial hypertension (PAH) (p< 0.0001), interstitial lung disease (ILD) (p=0.01), pulmonary fibrosis (p< 0.0001), and elevated CK (p< 0.01), received significantly more frequently DMARDs and/or IS than others. When comparing MCTD patients who evolved to a differentiated CTD (MCTD-dCTD, n=86; 27%) to patients who remained classified as MCTD, MCTD-dCTD patients were less frequently treated with HCQ (± CS) (23 (27%) vs 144 (46%), p< 0.0001) and were more often treated with a DMARD and/or IS (61 (71%) vs 100 (44%), p< 0.0001). At LFU, they were less frequently treatment-free (7 (8%) vs 51 (22%), p< 0.01) and received higher doses of CS (median dose of 7.5 [5-10] vs. 5 [5-10] mg/day, p=0.004) than MCTD patients. Development of ILD and/or PAH, as well as ILD alone, was associated with a less frequent use of HCQ at baseline (p< 0.05) (Table 3).
Conclusion: Treatments prescribed in patients with MCTD reflect the wide spectrum of the disease. HCQ and CS are cornerstones of the treatment and are sufficient in nearly half of MCTD patients, reflecting the good prognosis of this disease. MCTD-dCTD patients more often require DMARDs or IS. This work suggests that HCQ could prevent the development of life-threatening complications in MCTD.
1. Chevalier K, et al. J Intern Med. 2023
To cite this abstract in AMA style:
Chevalier K, Thoreau B, Michel M, Godeau B, AGARD C, Papo T, Sacré K, Seror R, Mariette X, Cacoub P, Benhamou Y, Levesque H, Goujard C, Lambotte O, Bonnotte B, SAMSON M, Ackermann F, Schmidt J, Duhaut P, Kahn J, Hanslik T, Costedoat-chalumeau N, Terrier B, Régent A, Dunogue b, cohen P, LE GUERN V, Hachulla E, Mouthon L, Chaigne B. Therapeutic Strategy in Patients with Mixed Connective Tissue Disease: A Multicenter Retrospective Study in the French MCTD Cohort [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/therapeutic-strategy-in-patients-with-mixed-connective-tissue-disease-a-multicenter-retrospective-study-in-the-french-mctd-cohort/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/therapeutic-strategy-in-patients-with-mixed-connective-tissue-disease-a-multicenter-retrospective-study-in-the-french-mctd-cohort/