Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Microvascular changes represent a key step of pathogenic process in Systemic Sclerosis (SSc). However, SSc has been demonstrated to carry an increased risk of cardiovascular diseases (HR 3.59), including peripheral artery disease1. Noteworthy, lower extremities arterial disease (LEAD) has been reported with increased frequency in patients with specific risk factors2 (digital ulcers, smoking, pulmonary arterial hypertension, corticosteroids) and also showed peculiar features on angiography in a small case series3.
Our aim was the estimation of LEAD prevalence in: (i) a cross-sectional analysis of our SSc cohort; (ii) at-risk SSc patients.
Methods: Consecutive SSc patients (ACR/EULAR 2016 criteria) attending our Centre for scheduled visits (October 2022-March 2024) were included. Patients without known LEAD and presenting ≥1 risk factor (PAH, digital ulcers, smoking current or stopped < =3 years, chronic steroids exposure PDN >=5 mg/day), were referred for lower extremities arterial Doppler ultrasonography (DUS) performed by an expert vascular surgeon. LEAD was classified according to Leriche-Fontaine stages.
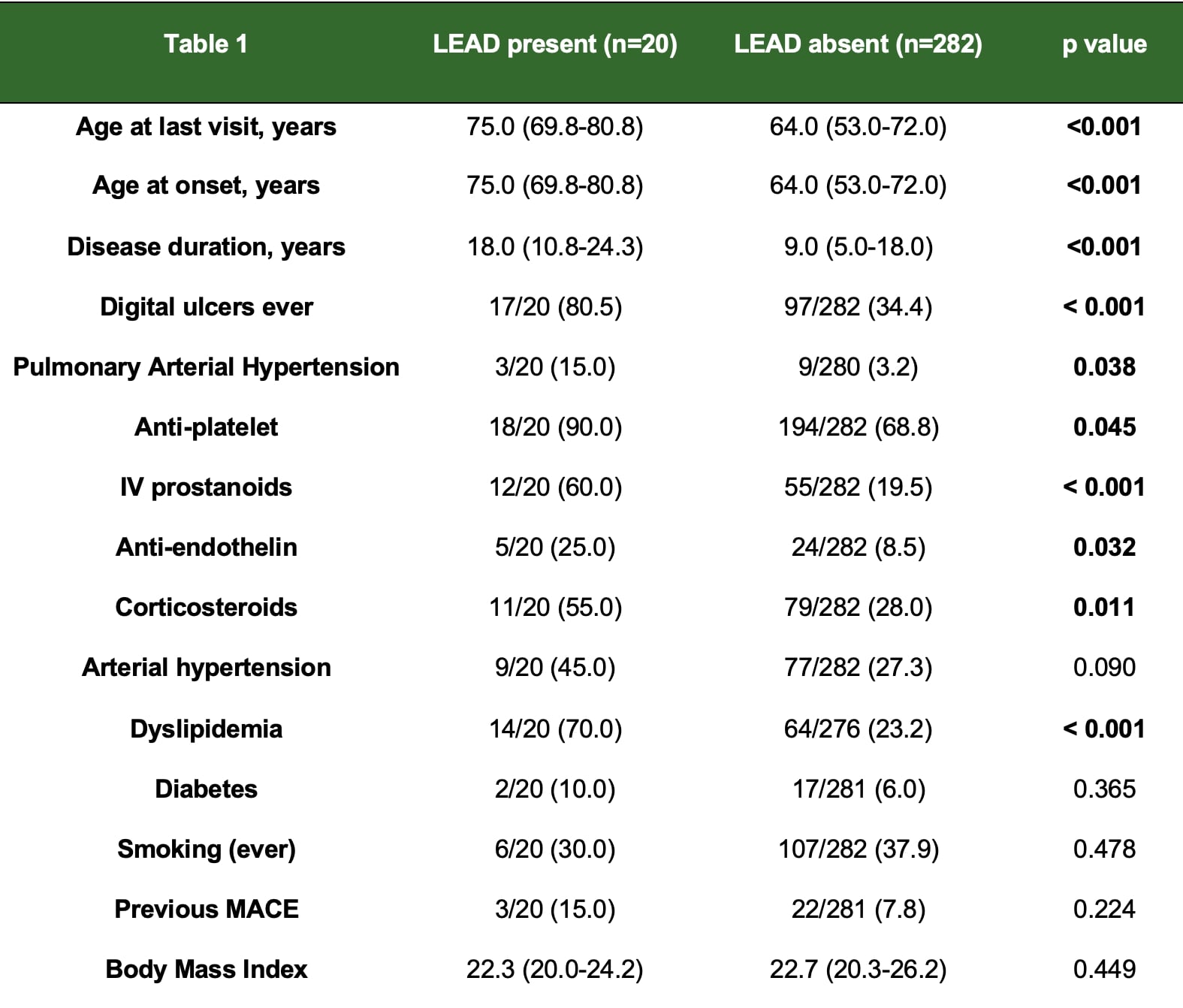
Results: Among 302 SSc patients evaluated in the indicated period (93% females, 85% limited cutaneous involvement, 51% anti-centromere+), 20 (6.6%) were previously diagnosed with LEAD, requiring revascularization interventions in 9 (45%) and amputations in 5 (25%). As compared to the remaining 282, they had higher age at onset and disease duration, higher rate of digital ulcers, PAH, comorbidities including major cardiovascular event (MACE) and more frequently received vasoactive treatments and steroids (Table 1).
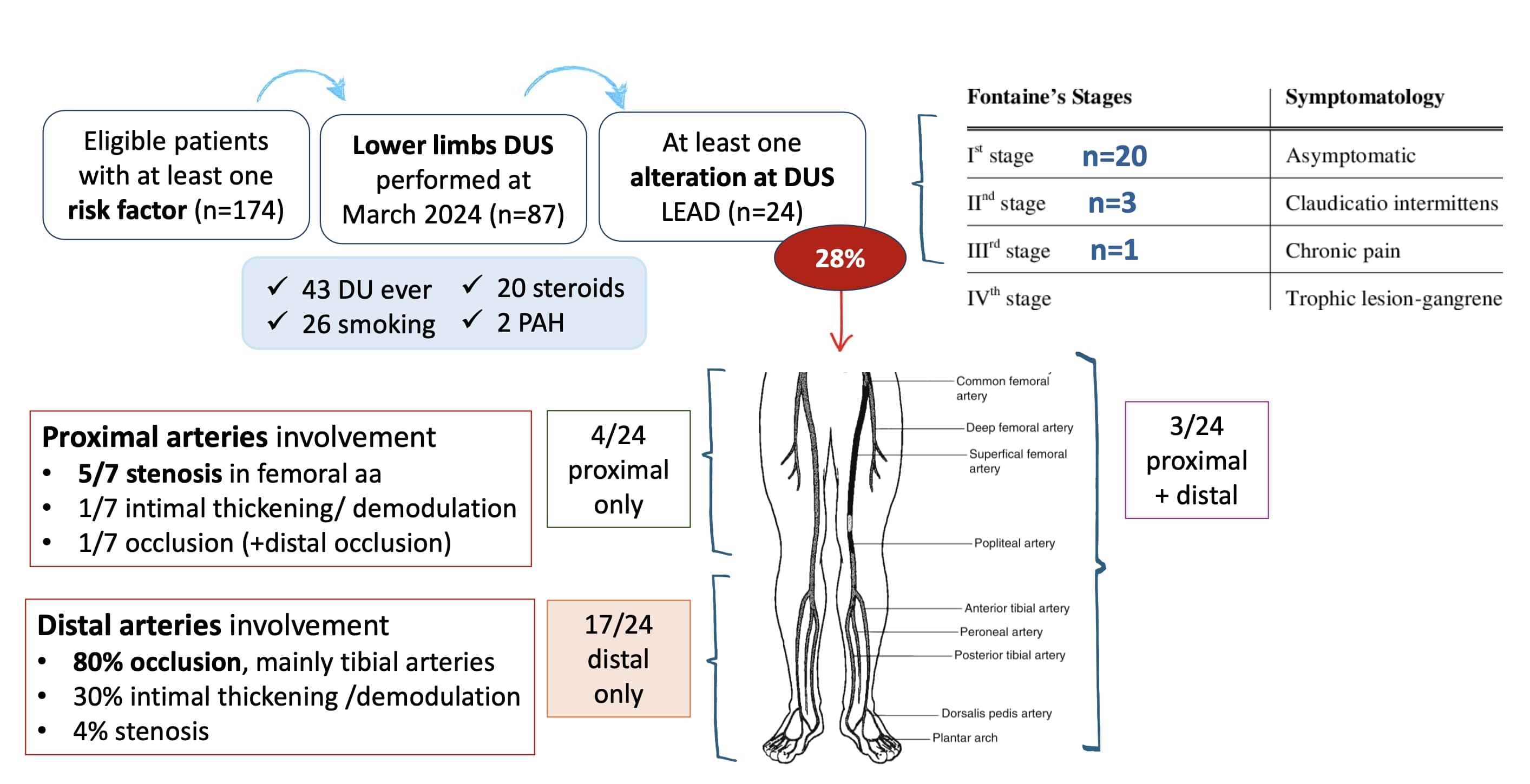
At least 1 LEAD risk factor was identified in 174/276 (63%) patients without known LEAD (Figure 1). Among them, 87/174 received DUS, with detection of LEAD in 24 (28%), classified as 20 stage I, 3 stage II and 1 stage III and characterized by distal arteries occlusion 20/24 patients.
Anti-platelet/anti-coagulant therapy was already ongoing in 17/24, while in the remaining 7 low dose aspirin was added. One patient with stage III was referred to angiographic study and underwent revascularization.
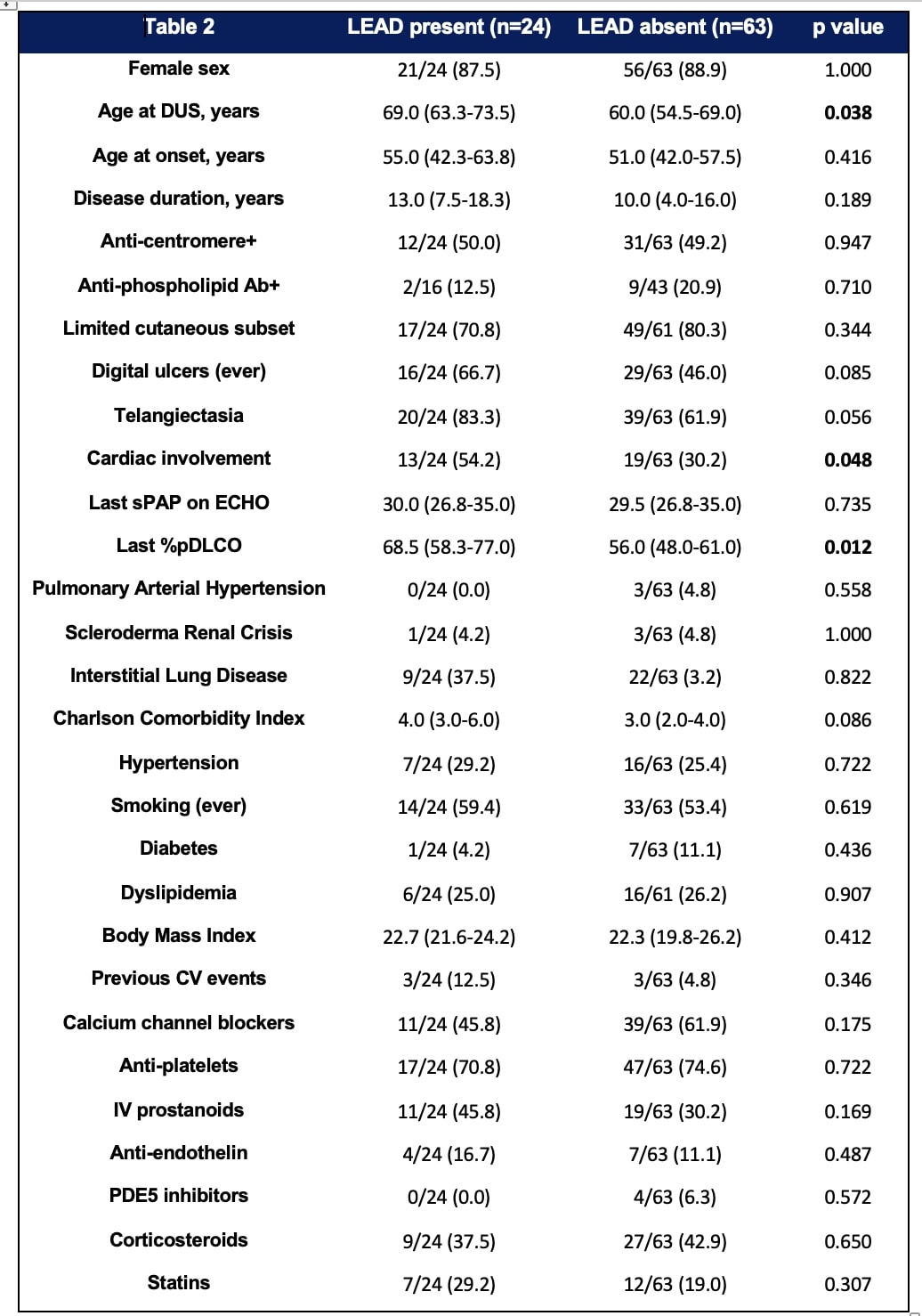
The comparison of patients with and without LEAD is shown in Table 2; multivariable logistic regression model confirmed lower %pDLCO (OR 6.25, 95%CI 1.84-21.2; p:003) and cardiac involvement (OR 4.43; 95% CI 1.20-16.3; p:0.024) as factors independently associated with LEAD, while smoking (ever) and age were not.
Conclusion: In the cross-sectional analysis of our SSc cohort, 6.6% had previous LEAD diagnosis, with 3% requiring a surgical procedure. Preliminary data on screening of at-risk patients showed LEAD at DUS in nearly one third, mostly asymptomatic, but with a specific pattern of distal arteries occlusion, without a strong association with traditional cardiovascular risk factors. Multidisciplinary discussion with a dedicated vascular surgeon is crucial to improve diagnosis and management of these patients.
REFERENCES. 1 Conrad N, Lancet 202;2 2 Yeo J, Nat Sci Rep 2022;3 Bertolino JSRD 2020
AKNOWLEDGEMENTS. The Authors thanks GILS (Gruppo Italiano Lotta Sclerodermia) for substantially supporting this project
To cite this abstract in AMA style:
Lazzaroni M, Baggi P, Moschetti L, Pedretti E, Piovani E, Barison C, Manzoni E, Franceschini F, Bonardelli S, Airò P. Prevalence and Risk Factors of Lower Extremities Arterial Disease in Systemic Sclerosis: Preliminary Data from a Single Centre Multidisciplinary Study [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/prevalence-and-risk-factors-of-lower-extremities-arterial-disease-in-systemic-sclerosis-preliminary-data-from-a-single-centre-multidisciplinary-study/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-and-risk-factors-of-lower-extremities-arterial-disease-in-systemic-sclerosis-preliminary-data-from-a-single-centre-multidisciplinary-study/