Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Pulmonary lung disease represents the most prevalent extra-glandular manifestation in patients with Sjögren’s syndrome (SS). Notably, interstitial lung disease (ILD) stands out as the most severe pulmonary complication. Recent studies show a pooled SS–ILD prevalence of around 23%. Research on ILD and SS is limited, and there is a lack of information regarding the proportion of patients who experience progressive pulmonary fibrosis (PPF) during follow-up.
Methods: A descriptive and prospective study was performed using a cohort of patients with SS and ILD collected from a collaborative Rheumatology-Pulmonology clinic. Patients who met the 2016 ACR/EULAR criteria for SS and had a diagnosis of ILD on computed tomography (CT) were recruited prospectively. Sociodemographic and clinical data were collected. During follow-up, dyspnea progression, pulmonary function test (forced vital capacity [FVC], diffusion capacity for carbon monoxide [DLCO]), and computed tomography findings were monitored. Progressive pulmonary fibrosis (PPF) was defined according to the ATS/ERS/JRS/ALAT criteria.
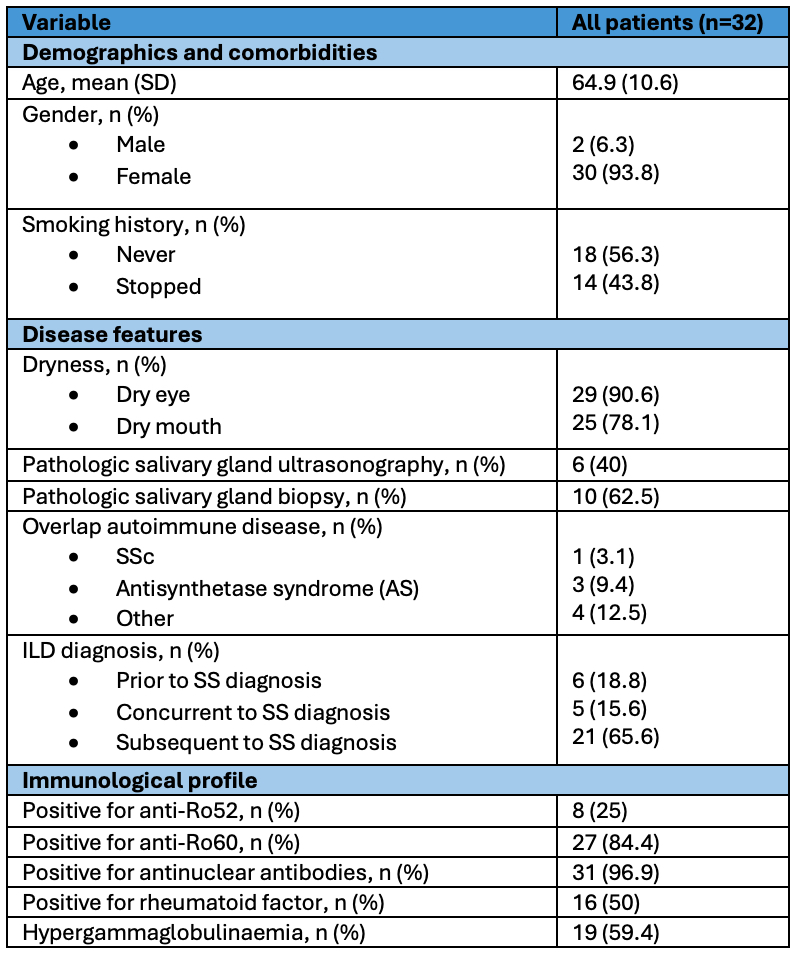
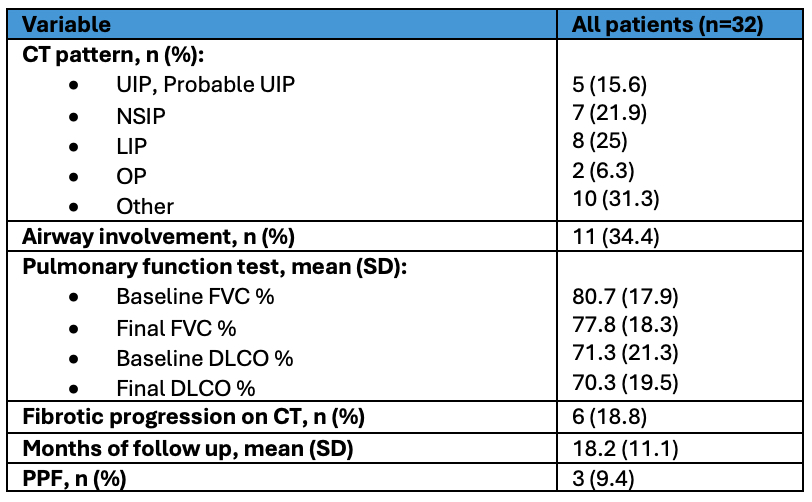
Results: A total of 32 subjects diagnosed with SS-ILD were included. Demographics and baseline characteristics are shown in Table 1. The mean follow-up time in the collaborative clinic was 18.2 months. Most patients had non-specific interstitial pneumonia (NSIP) or lymphoid interstitial pneumonia (LIP) patterns, and approximately one-third had concomitant airway involvement. The different patterns of involvement and their progression are presented in Table 2.
Extrapulmonary manifestations were common in this cohort. The most frequent manifestations were Raynaud’s phenomenon (18.8%), peripheral nervous system involvement (9.4%), and arthritis (9.4%). A total of 6 patients (18.8%) had concomitant neoplasia, half of which were hematologic.
Half of the patients were receiving corticosteroid therapy at the baseline visit. The most frequent immunosuppressive therapies were azathioprine (21,9%) and rituximab (21,9%), followed by methotrexate (15.6%) and mycophenolate (12.5%). Additionally, one patient received tocilizumab (3.1%).
During the follow-up, only three patients met the criteria for PPF. Two of these patients had a fibrotic NSIP pattern, while the third presented a usual interstitial pneumonia (UIP) pattern. Only two patients received treatment with nintedanib, with one requiring discontinuation due to adverse effects (diarrhea and weight loss). There were no hospitalizations for acute exacerbations or deaths.
Conclusion: In our cohort of patients with SS and ILD, the majority demonstrated functional and radiological stability during follow-up. Only 9.4% of the patients met the criteria for PPF, and there were no acute exacerbations or deaths. However, larger cohorts and longer follow-ups are needed to confirm these findings.
To cite this abstract in AMA style:
Jiménez Barrios S, Garrote Corral S, Rigual J, de La Puente Bujidos C, Blazquez Canamero M, Loarce J. Sjögren’s Syndrome and Interstitial Lung Disease: Experience in a Collaborative Rheumatology-Pulmonology Clinic [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/sjogrens-syndrome-and-interstitial-lung-disease-experience-in-a-collaborative-rheumatology-pulmonology-clinic/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/sjogrens-syndrome-and-interstitial-lung-disease-experience-in-a-collaborative-rheumatology-pulmonology-clinic/