Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Metformin (Met) is a widely used, first-line antidiabetic drug with AMPK-dependent anti-inflammatory and immunomodulatory effects. In in vitro studies and human trials in SLE and multiple sclerosis, Met associates with a reduction of Th17 cells and of IL-17, IL-1b, IL-6, IFN-g, and TNF-a levels, while restoring or increasing regulatory T cell (Treg) levels. Sjögren’s Disease (SjD) is a systemic autoimmune disorder characterized by autoantibody production and lymphocytic infiltration of the exocrine glands. In SjD, T cells participate in target organ inflammation and promote B cell activation; it has been proposed that an imbalance between pro-inflammatory Th17 and T follicular helper cells and their regulatory counterparts, Treg and T follicular regulatory cells, is a key component of pathogenesis. Met-treated SjD mice showed improved salivary gland function and re-establishment of the T cell equilibrium. Based on this premise, we reviewed the impact of Met on SjD in two large independent SjD cohorts.
Methods: The clinical and serologic features of patients classified as SjD (ACR-EULAR) in the OMRF cohort were retrospectively reviewed. Cases were defined as SjD diabetic patients treated with Met (SjD-Met) at the time of evaluation (n=31). The comparison groups were 1) SjD non-diabetic, not on Met matched by age, sex, and race 1:4 to the cases (SjD-match, n=124); 2) SjD diabetic patients not treated with Met (SjD-DM-notMet, n=59); 3) All diabetic SjD, irrespective of treatment (SJD-DM, n=84); and 4) All non-diabetic SjD in the cohort (SjD-nonDM, n=375). Similar analyses were conducted in a replication cohort (NIDCR; SjD-Met (n=26) and SjD-nonDM (n=394)) and the results combined in a meta-analysis.
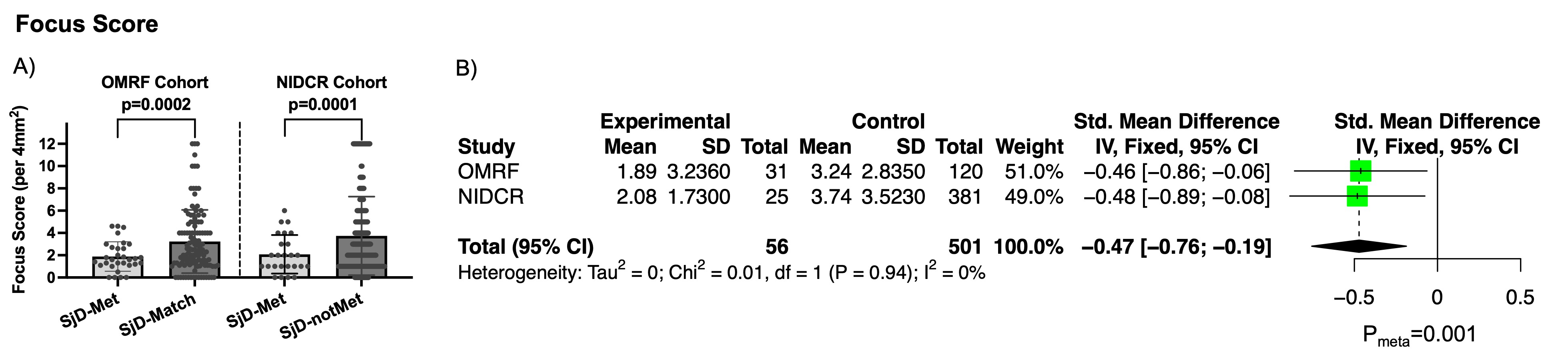
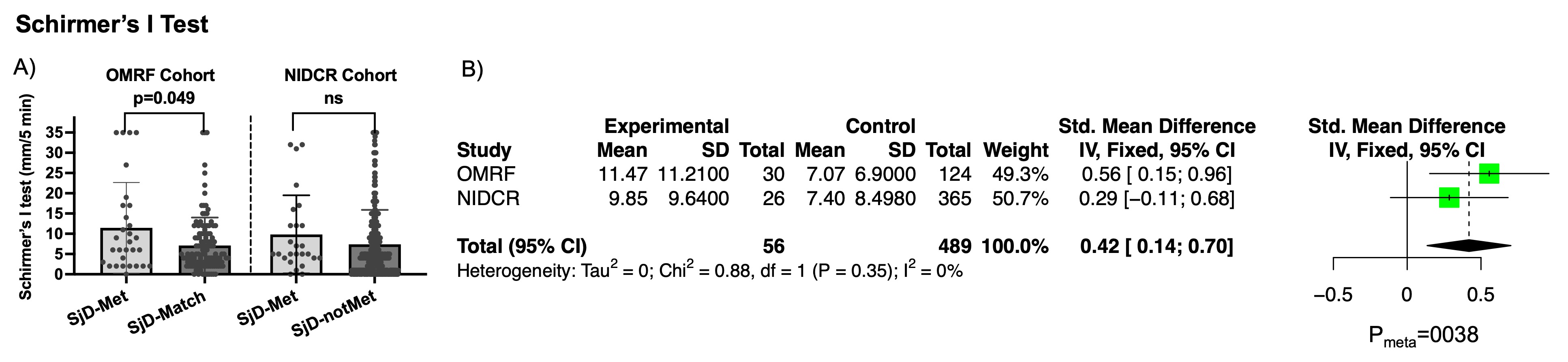
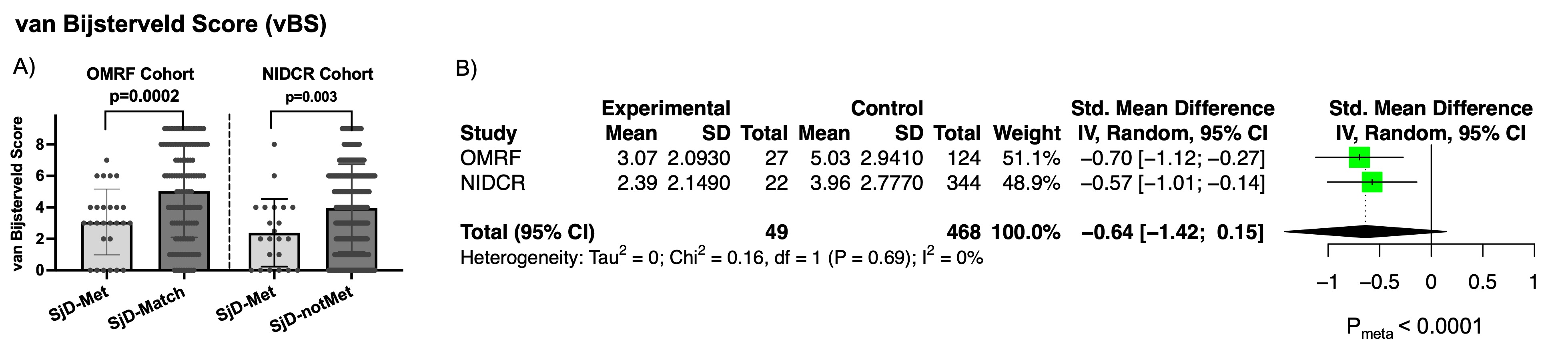
Results: No significant differences in sociodemographic features were observed across groups. In the OMRF discovery cohort, SjD-Met had lower salivary gland focus scores than SjD-match (1.88±1.32 vs. 3.26±2.91, p=0.0002) despite similar unstimulated salivary flow rates. These findings were replicated in the NIDCR cohort (p=0.0001) and the meta-analysis (SD mean D -0.47 [-0.76; -0.19]; p=0.001) (Fig. 1). OMRF-SjD-Met subjects had lower rates of (+) Schirmer’s and vBS than SjD-match (OR 0.40, p=0.028; and OR 0.24, p=0.004, respectively); findings were replicated in the NIDCR cohort and meta-analysis (p=0.0038 for Schirmer’s and p< 0.0001 for vBS) (Figs. 2 and 3). This pattern persisted when SjD-Met was compared to SjD-DM-notMet but the effects disappear when comparing all diabetics to non-diabetics, linking the effects with Met. The only differences that could be attributed to diabetes, since they were observed when comparing all diabetics (irrespective of treatment) to non-diabetics, were lower salivary flow volumes and higher ESR in SjD-DM (OMRF cohort).
Conclusion: Our retrospective study of two independent SjD cohorts show that SjD patients receiving Met have less extensive focal lymphocytic infiltration of the minor salivary glands and lower rates of abnormal ocular tests (Schirmer’s and vBS) than their counterparts not on Met. These results justify the design of prospective, randomized, double-blind trials of Met, an accessible and safe drug for SjD, a disease with great unmet therapeutic needs.
To cite this abstract in AMA style:
Rasmussen A, Baer A, Grader-Beck T, Beach M, Warner B, Lessard C, Farris A, Scofield R. Metformin Improves Salivary Gland Infiltration and Objective Measures of Dry Eyes in Sjögren’s Disease: A Retrospective Observational Study [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/metformin-improves-salivary-gland-infiltration-and-objective-measures-of-dry-eyes-in-sjogrens-disease-a-retrospective-observational-study/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/metformin-improves-salivary-gland-infiltration-and-objective-measures-of-dry-eyes-in-sjogrens-disease-a-retrospective-observational-study/