Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Frailty is a state of decreased physiological reserve that confers an increased vulnerability to stressors and adverse outcomes1. Compared to the general population, frailty occurs at a younger age in RA2, and the prevalence of frailty is higher in Veteran populations3. Fried Frailty Phenotype (FFP)1, FRAIL Scale (FRAIL)4, and VA Frailty Index (VAFI)3 are validated tools that use either a phenotype (FFP, FRAIL) or deficit accumulation approach (VAFI). Each has been studied in RA; however, they have not all been measured in a single RA cohort. This study aims to compare the agreement of these three frailty instruments.
Methods: Data were from the VA Rheumatoid Arthritis Frailty and Osteoporosis (VA-FROst) single center longitudinal cohort. Participants met the 2010 ACR RA classification criteria and were ³35 years old. FFP measured fatigue, physical activity, weight loss, hand grip strength (HGS) and walking speed1. FRAIL queried patient-reported fatigue, ability to climb stairs, walk moderate distances, presence of ³5 illness, and weight loss4. VAFI used electronic health record (EHR) diagnostic codes to inform 31 deficit categories based on morbidities, cognition/mood, sensory and functional impairments, and other/geriatric syndromes3. The VAFI is a ratio of the number of deficits divided by the total. Each frailty instrument categorized individuals as robust, pre-frail or frail1,3,4. We examined subcomponents contributing to each frailty instrument. Percent agreement and kappa tests evaluated accordance between instruments.
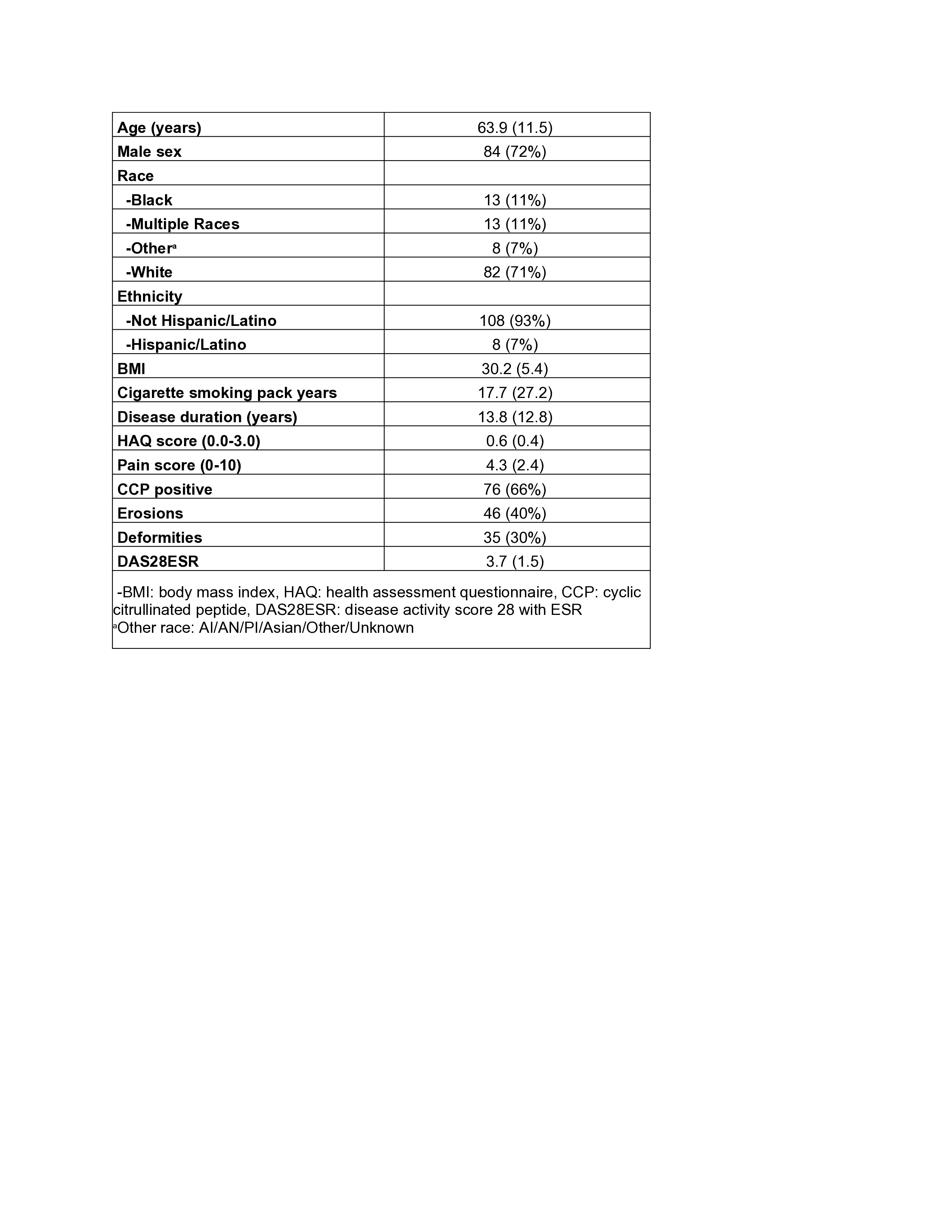
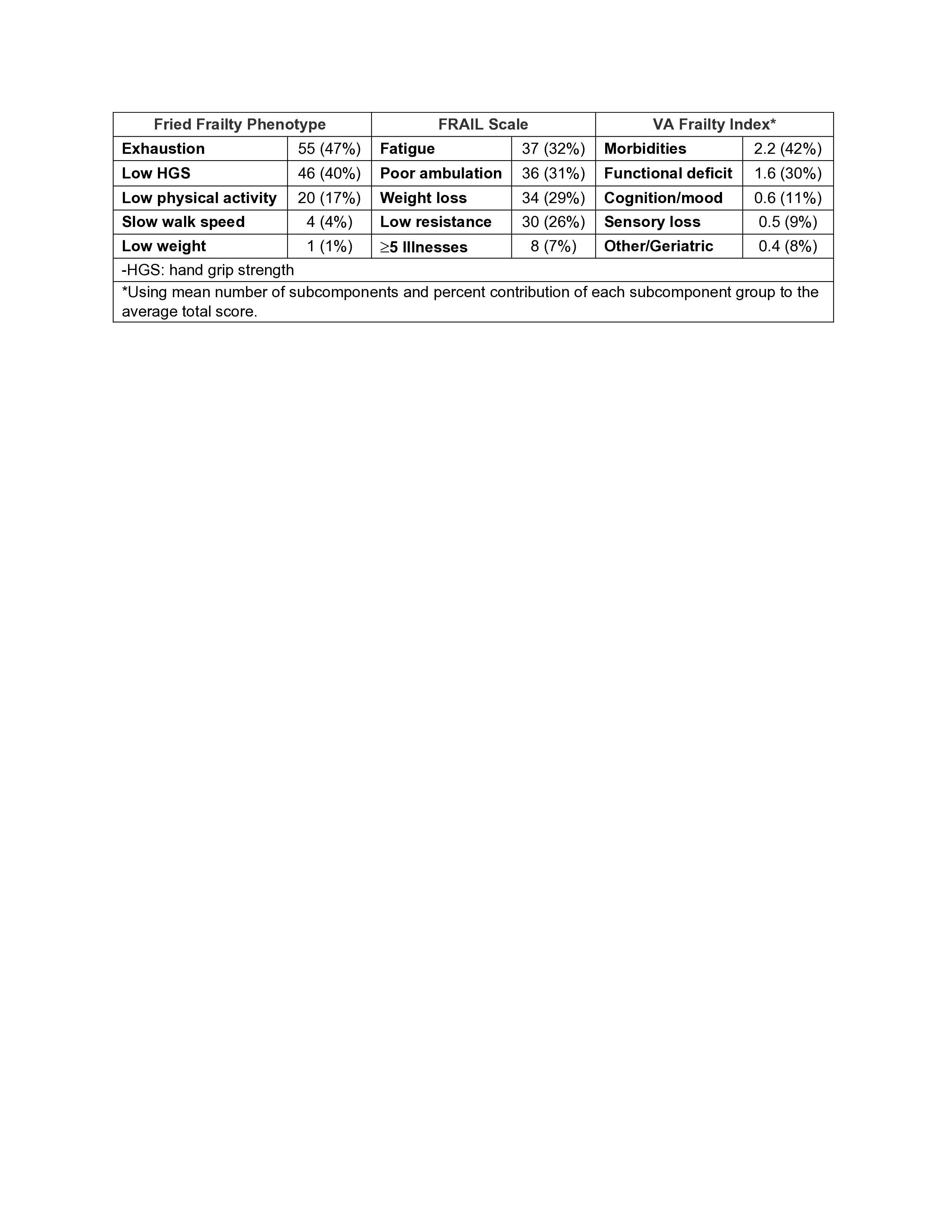
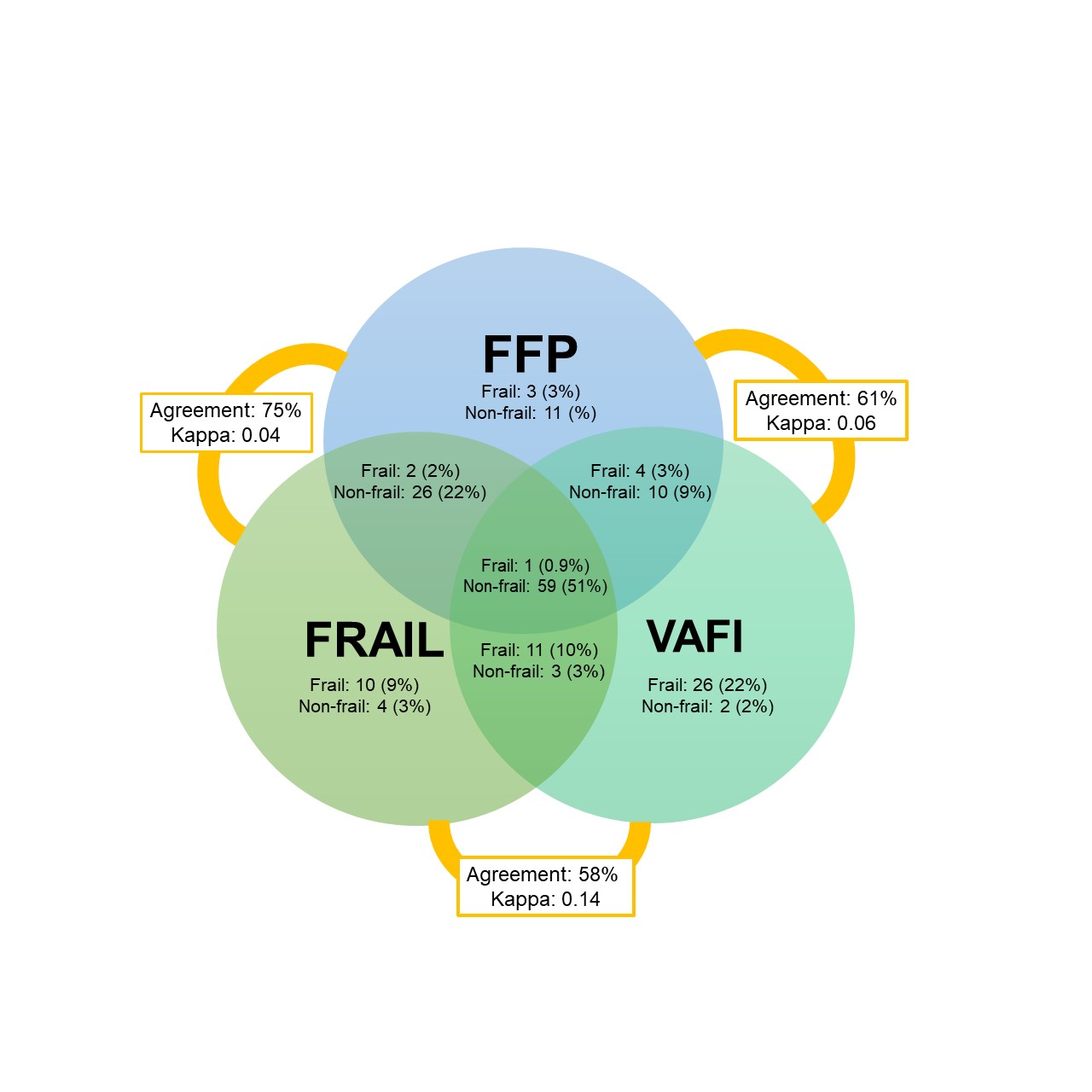
Results: We studied 116 Veterans aged 63.9±11.5, 84 (72%) participants were male, and 13 (11%) were Black (Table 1). Disease duration was 13.8±12.8 years, anti-CCP positivity was present in 76 (66%), and disease activity was moderate on average (DAS28ESR 3.7±1.5). Compared to the other instruments, VAFI categorized the most participants as frail (n=42, 36%), followed by FRAIL (n=24, 21%), and FFP (n=9, 8%) (Figure 1). Exhaustion (47%) and low HGS (40%) were the most common FFP deficits (Table 2). All FRAIL subcomponents had similar frequencies (26-32%) with exception of ≥5 illnesses (7%). VAFI score was primarily driven by morbidities (42%) and functional deficits (30%). One (1%) Veteran was frail by all instruments, 17 (15%) were frail by 2 instruments. The frailty instruments demonstrated moderate percent agreement (58%-75%) and poor agreement by kappa testing (k 0.04-0.14) (Figure 1).
Conclusion: In our cohort of Veterans with RA, measuring frailty by the FFP, FRAIL, and VAFI showed low agreement by kappa testing. This incongruence is likely due to differences in the way frailty is conceptualized (phenotype vs. deficit accumulation) and assessed (patient-report, direct assessment, EHR). Further studies comparing the predictive capacity of long-term health outcomes between frailty instruments are needed to better understand these differences.
- Fried L et al. J Gerontol A Biol Sci Med Sci 2001
- Loecker C et al. ACR Open 2023
- Orkaby AR et al. J Gerontol A Biol Sci Med Sci 2019
- Van Kan GA et al. J Am Med Dir Assoc 2008
To cite this abstract in AMA style:
Riggles K, Brubeck H, Bass R, Loecker C, Roul P, England B, Wahl E, Andrews J, Singh N, Baker J, Katz P, Shoback D, Garcia J, orkaby a, Wysham K. Assessing the Performance of Validated Frailty Instruments in Veterans with Rheumatoid Arthritis (RA) [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/assessing-the-performance-of-validated-frailty-instruments-in-veterans-with-rheumatoid-arthritis-ra/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/assessing-the-performance-of-validated-frailty-instruments-in-veterans-with-rheumatoid-arthritis-ra/