Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Juvenile myositis (JM) patients experience a high burden of emotional distress, yet mental health (MH) care is not typically integrated into standard clinical practices. Unaddressed MH issues can adversely affect patients’ quality of life and disease outcomes. As part of a quality improvement initiative to implement MH screening and integrated, onsite social work (SW) within the SickKids JM clinic, this study aimed to 1) investigate the relationship between patient/parent and physician global assessments (PPGA and PGA) and patients’ MH screens, and 2) describe the outcomes of integrated SW support for JM patients.
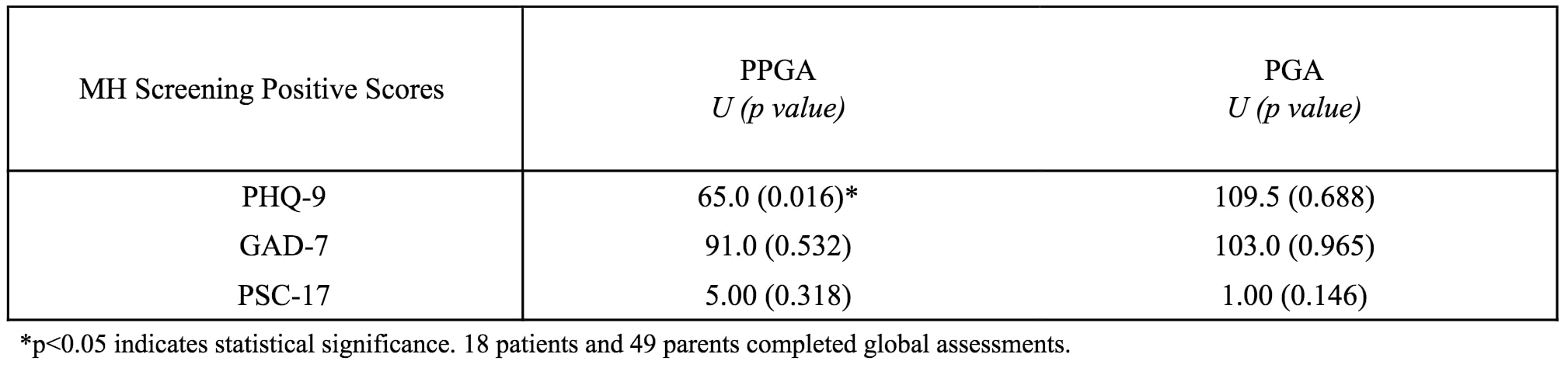
Methods: We screened JM patients at clinic visits from January 2023-2024 using parent proxy Pediatric Symptom Checklist-17 (PSC-17) for ages 5-11 years, and the Patient Health Questionnaire-9 (PHQ-9) and General Anxiety Disorder-7 (GAD-7) for ages 12-18 years. Patients with positive screens, total score above established cutoffs, were offered a real-time SW referral, including same-day introduction and an initial SW session scheduled within a week. PPGA and PGA scores were routinely collected during visits. The relationship between global scores and baseline MH screening scores was analyzed using Mann-Whitney U test. We used descriptive statistics to tabulate screening data and qualitatively characterized SW activities including MH issues addressed and interventions provided.
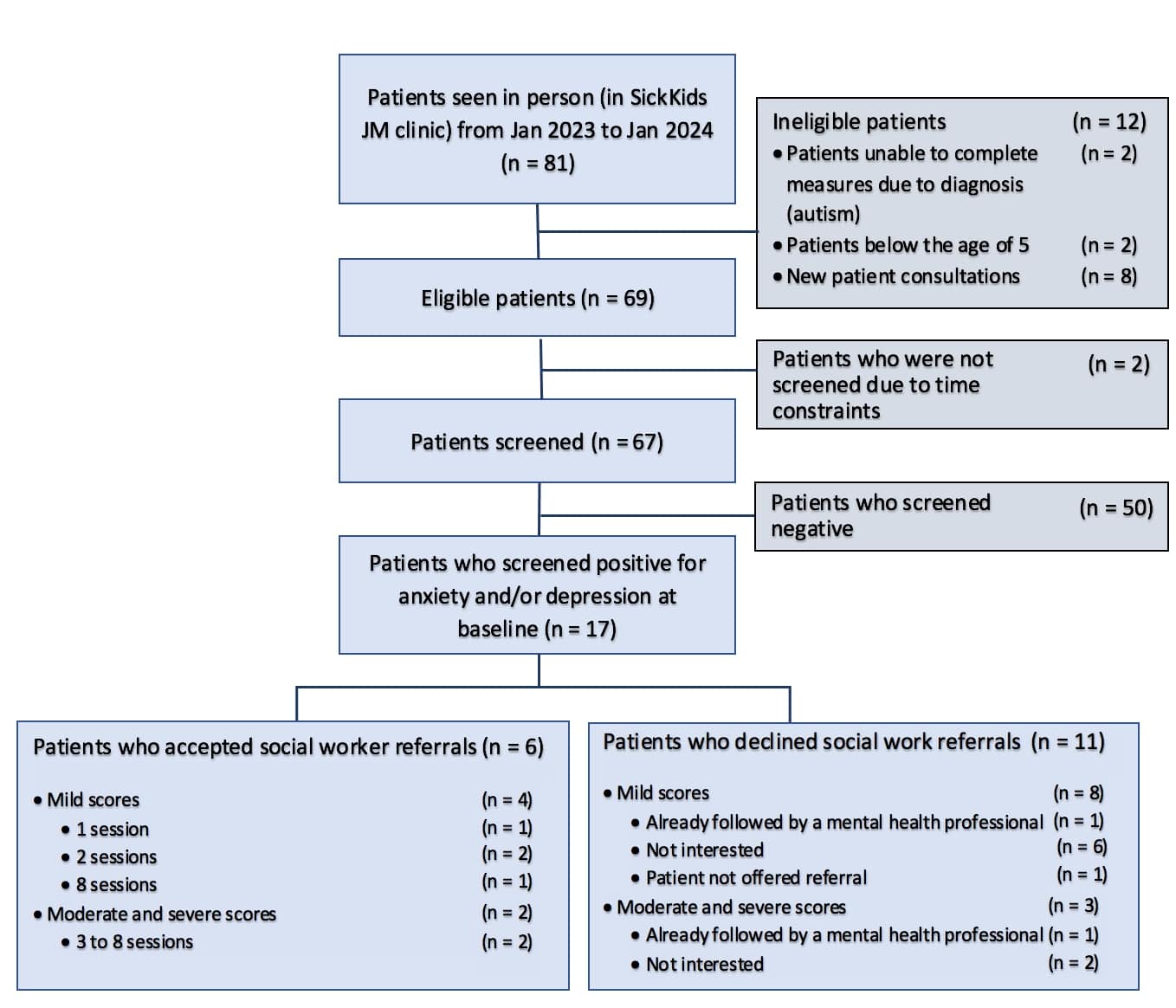
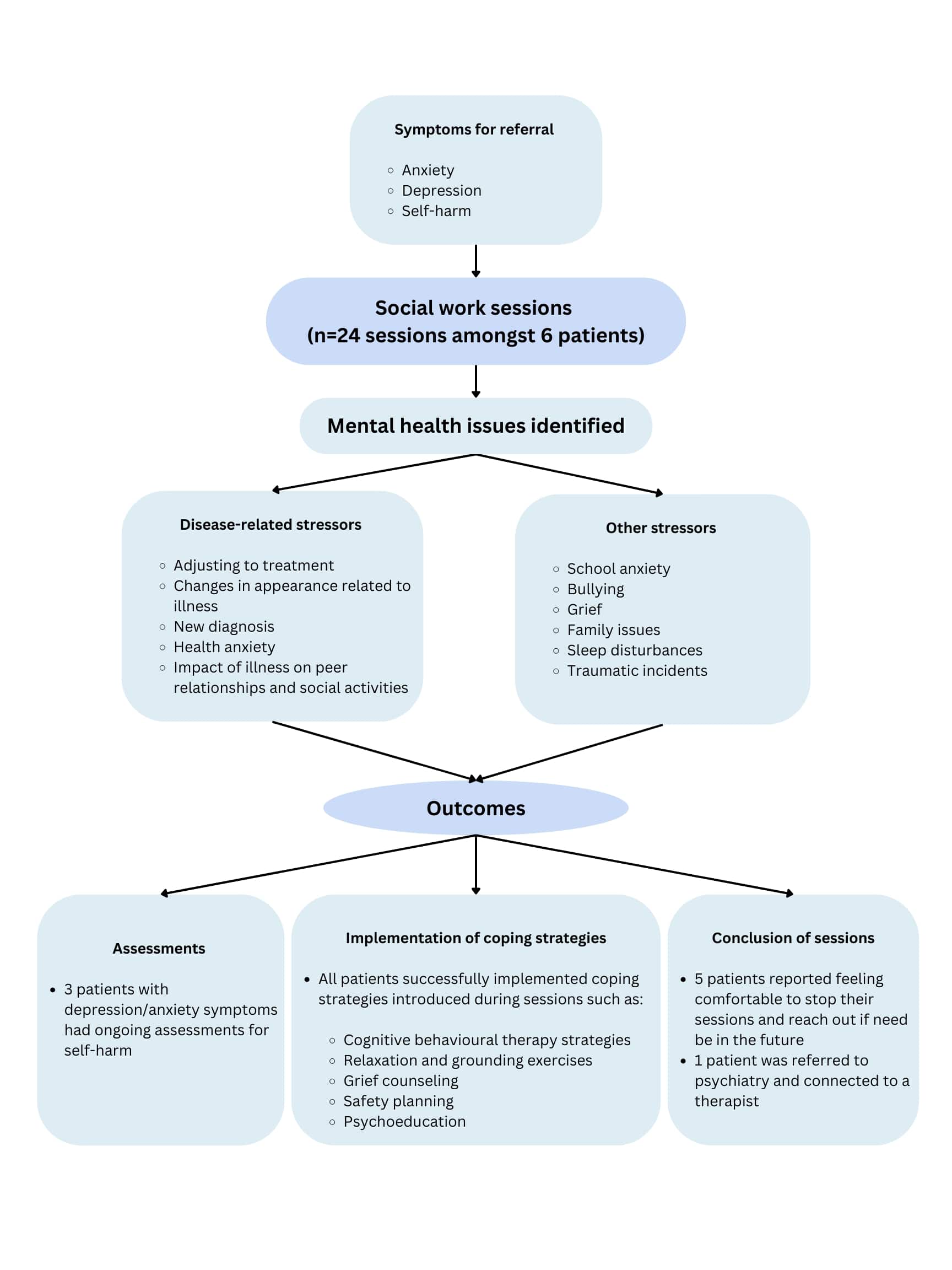
Results: MH screens were completed for 67 patients, with 46 females (69%) and a mean age of 12.4 years (SD=3.3). Seventeen patients (25%) screened positive at baseline (Figure 1), including three reporting passive suicidal ideation. Higher PPGA was significantly associated with positive PHQ-9 screens (U=65.0 p=0.016). No significant associations were observed between any positive MH screens and PGA (Table 1). Of the 17 patients with positive screens, 6 (35%) accepted SW referrals. Comparing those accepting to those declining referrals, the median age was 15.6 (IQR=3.2) vs 13.5 (IQR=2.7) years, and symptom severity was similar with 33% vs 27% having moderate/severe scores (Figure 1). Over the one year, 24 1-hour sessions were conducted amongst the 6 referred patients. Patients reported their MH being affected by disease-related issues and other external stressors (Figure 2). Psychoeducation and counseling interventions tailored to patients’ needs were provided during sessions. Over the one-year period, patients successfully implemented learned skills and all but one concluded their sessions due to improved MH.
Conclusion: We successfully implemented and sustained a MH screening program with integrated SW intervention in the SickKids JM clinic. While PPGA may help identify prevalent MH symptoms, PGA alone may not reflect concerns, underscoring the need for routine MH screening in the JM population. Although only a small number of patients accepted referrals to integrated SW, sessions allowed patients to access appropriate interventions, and for the majority, improved their MH. The limited acceptance rate, predominantly by younger patients, highlights the need for enhanced psychoeducation to fully integrate MH care into routine clinic practices.
Patients seen in JM clinic included 58 patients with juvenile myositis, 6 patients with scleroderma, and 3 patients with overlap syndromes. On the PHQ-9 and GAD-7, screens were positive if scores were higher than 4; on the PSC_17, screens were positive if scores were higher than 15. On the PHQ-9, positive scores were interpreted as follows: 5-9 (mild), 10_14 (moderate), 15_19 (moderately severe) and 20_27 (severe). On the GAD-7, positive scores were interpreted as follows: 5-9 (mild), 10_14 (moderate) and 15_21 (severe). One patient with a mild score was not offered a referral by clinicians who determined the need for a referral to be assessed at follow-up.
To cite this abstract in AMA style:
Flores Pereira L, Boulard L, Baker K, Bell-Peter A, Carbone V, Feldman B, MacMahon J, Maniscalco V, Marcuz J, Slater T, Whitney K, Goh Y, Knight A. Implementing Integrated Mental Health Care in a Juvenile Myositis Clinic: A One-Year Review [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/implementing-integrated-mental-health-care-in-a-juvenile-myositis-clinic-a-one-year-review/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/implementing-integrated-mental-health-care-in-a-juvenile-myositis-clinic-a-one-year-review/