Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Children with juvenile dermatomyositis (JDM) and juvenile idiopathic arthritis (JIA) have impaired quality of life and increased rates of anxiety and depression (15-65%), even in disease remission, when compared to healthy children. Narrative medicine is a group-based intervention that allows patients to reconstruct medical experiences through written or oral self-reflective perspectives. It has demonstrated improved patient-reported outcomes with reduced rates of depression in adults but there is limited data in pediatric rheumatology. This explorative study assesses the feasibility of a patient-targeted narrative medicine intervention and its impact on mental health burden in JDM and JIA.
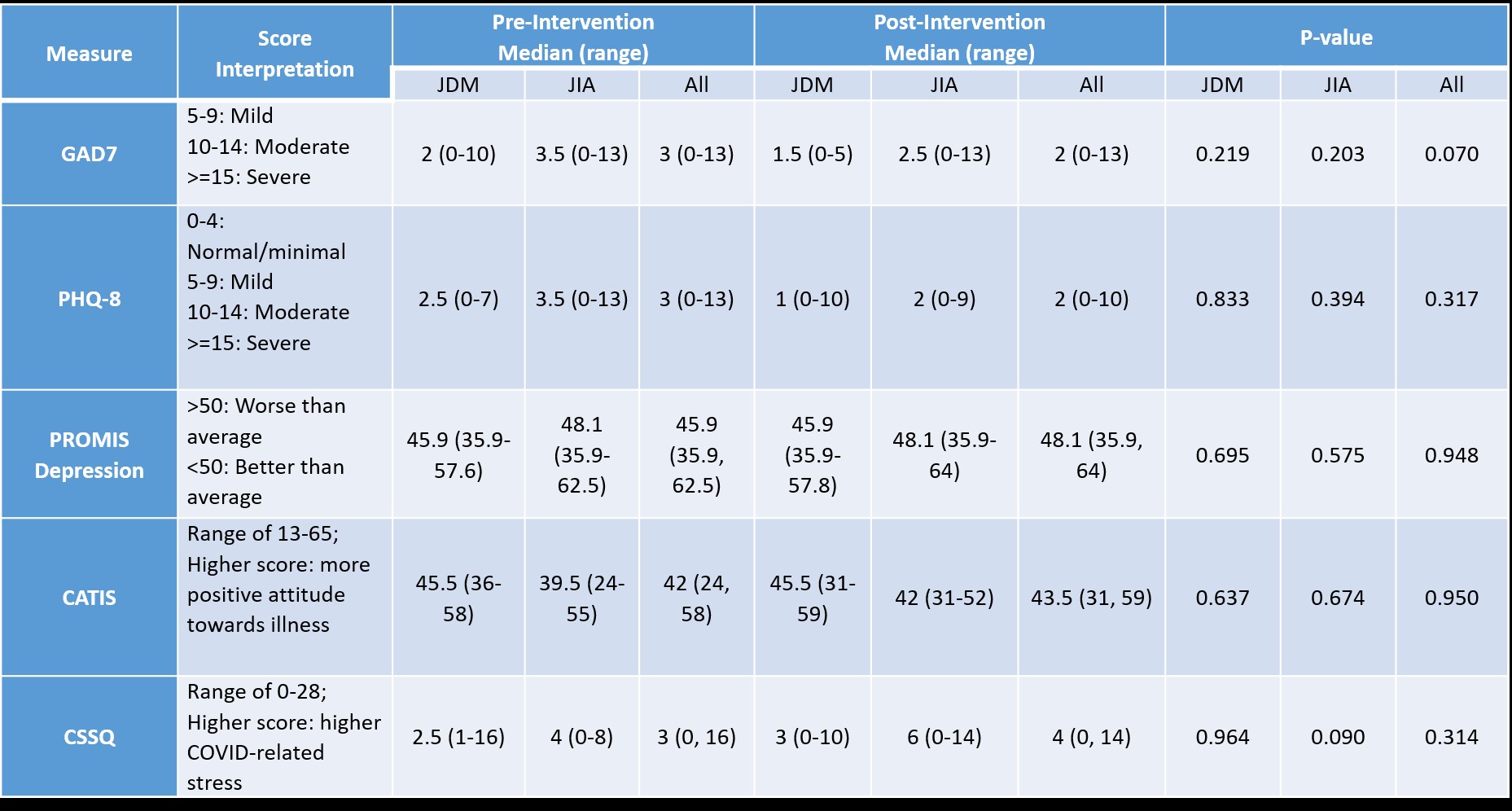
Methods: We prospectively recruited patients ages 6 to with JDM and JIA for a narrative medicine intervention. Participants were divided by diagnosis and age into four narrative medicine groups, with 4-6 patients per narrative medicine session. Six sessions were held over 3 months by two trained facilitators per group. Demographic and medical information were collected by chart review. To assess mental health, patients completed pre- and post-intervention questionnaires including Patient-Reported Outcomes Measurement Information System (PROMIS) Depression Scale, Generalized Anxiety Disorder-7 (GAD-7), Childhood Attitude Towards Illness Scale (CATIS), Patient Health Questionnaire-8 (PHQ-8), and CoVID Stress Scale (CSSQ).
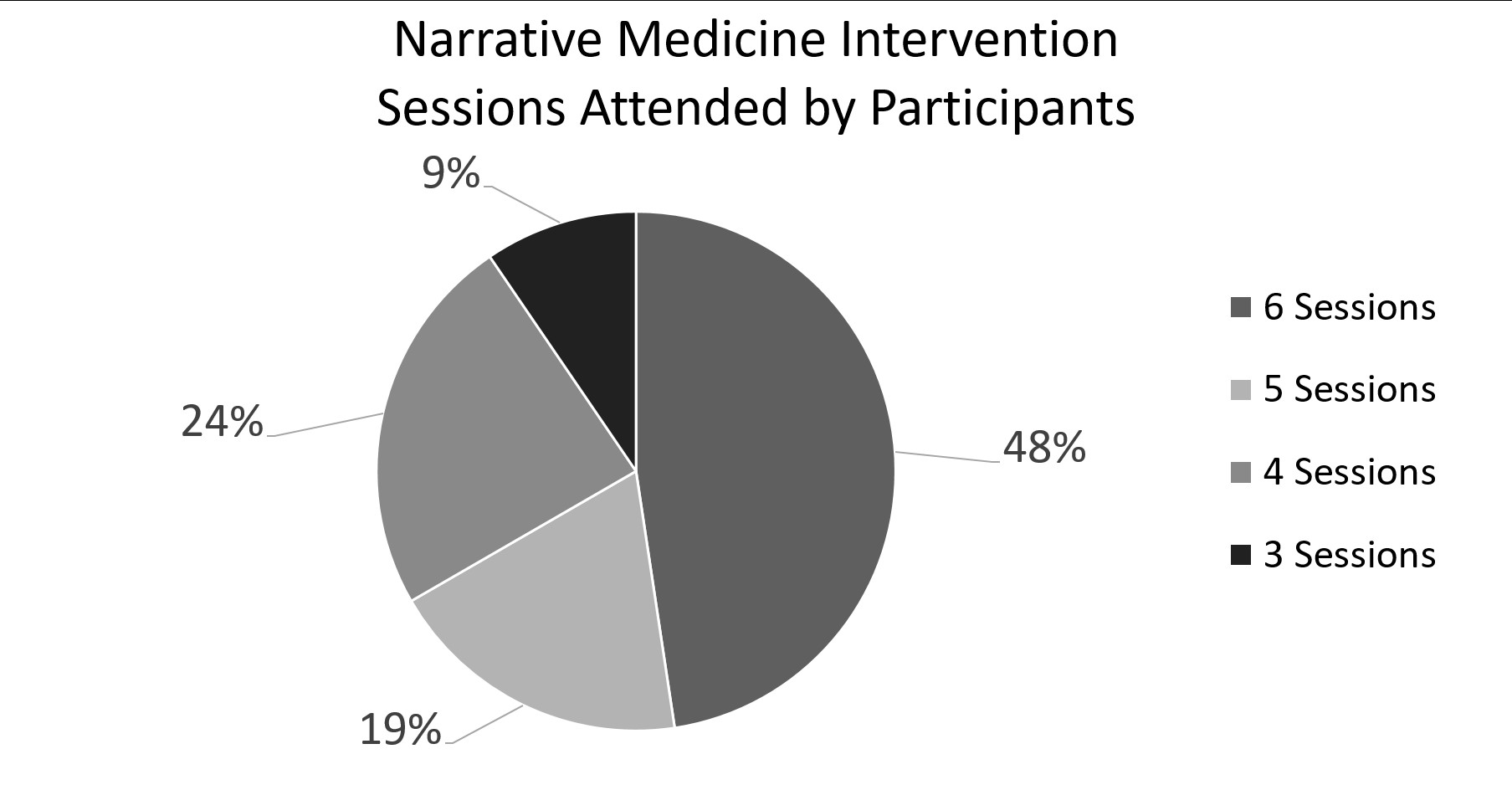
Results: Twelve patients with JDM (67 % female) and nine with JIA (78% female; 4 persistent oligoarticular JIA, 3 RF-negative, 1 psoriatic JIA and 1 enthesitis-related arthritis) participated in the narrative medicine intervention. All patients participated in at least 50% of sessions (Figure 1). Pre-intervention, 58% of patients with JDM and 67% of patients with JIA had inactive disease, while post-intervention 70% of patients with JDM and 55% of patients with JIA had inactive disease (Table 1). Wilcoxon signed-rank test revealed no statistically significant difference between pre- and post-intervention questionnaires for any of the scales. Sub-analysis of those with elevated GAD-7 and PHQ-8 pre-intervention showed trend towards improvement in anxiety (p=0.057) and no change for depression (p=0.171).
Conclusion: All patients participated in at least 50% of narrative medicine sessions, demonstrating feasibility. This exploratory study showed trend toward improved anxiety following narrative medicine session participation for those with elevated GAD7 but did not demonstrate significant changes in PHQ-8, PROMIS depression, CSSQ or CATIS scales likely due to small numbers and low level of mental health issues in those that participated in this study.
To cite this abstract in AMA style:
Lanis A, Steelquist E, Lood C, Shenoi S. Narrative Medicine Intervention for Mental Wellbeing in Juvenile Myositis and Juvenile Idiopathic Arthritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/narrative-medicine-intervention-for-mental-wellbeing-in-juvenile-myositis-and-juvenile-idiopathic-arthritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/narrative-medicine-intervention-for-mental-wellbeing-in-juvenile-myositis-and-juvenile-idiopathic-arthritis/