Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Patients with rheumatoid arthritis (RA) frequently visit the emergency department (ED). However, very little is known regarding the clinical characteristics of patients visiting the ED and the factors influencing their admission to the hospital from the ED. Our study aimed to investigate the epidemiology and outcomes of ED visits among patients with RA utilizing the Nationwide Emergency Department Sample (NEDS).
Methods: Using NEDS data from 2019, ED visits with diagnosis of RA were identified using ICD -10 codes M05.X or M06.X. Patient demographics, clinical features, and comorbidities were compared between RA and non-RA ED visits. Variations in ED visits by race categories were also assessed. Additionally, multivariable logistic regression analysis was used to examine factors linked to inpatient admission from the ED. We also assessed the top diagnoses associated with ED visits in each group.
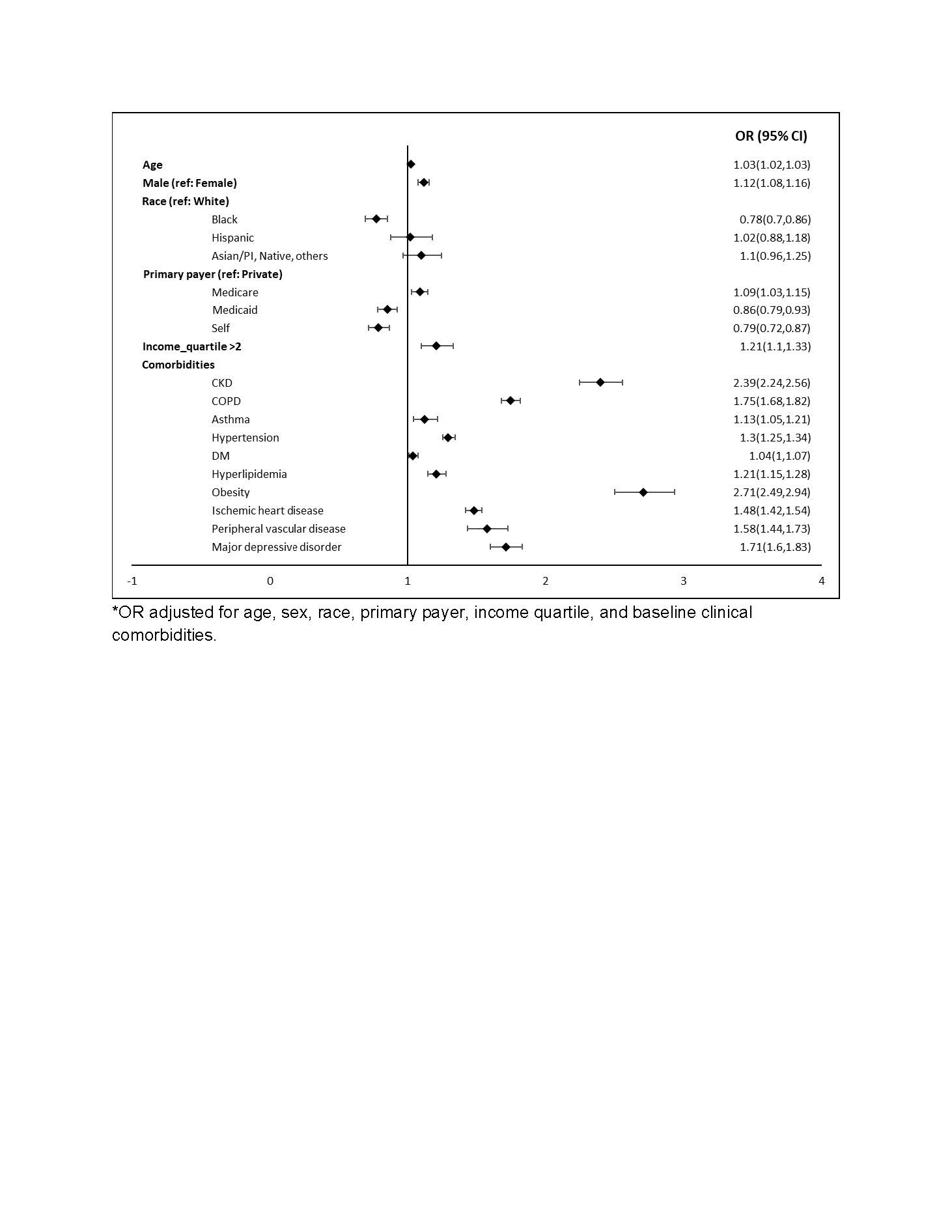
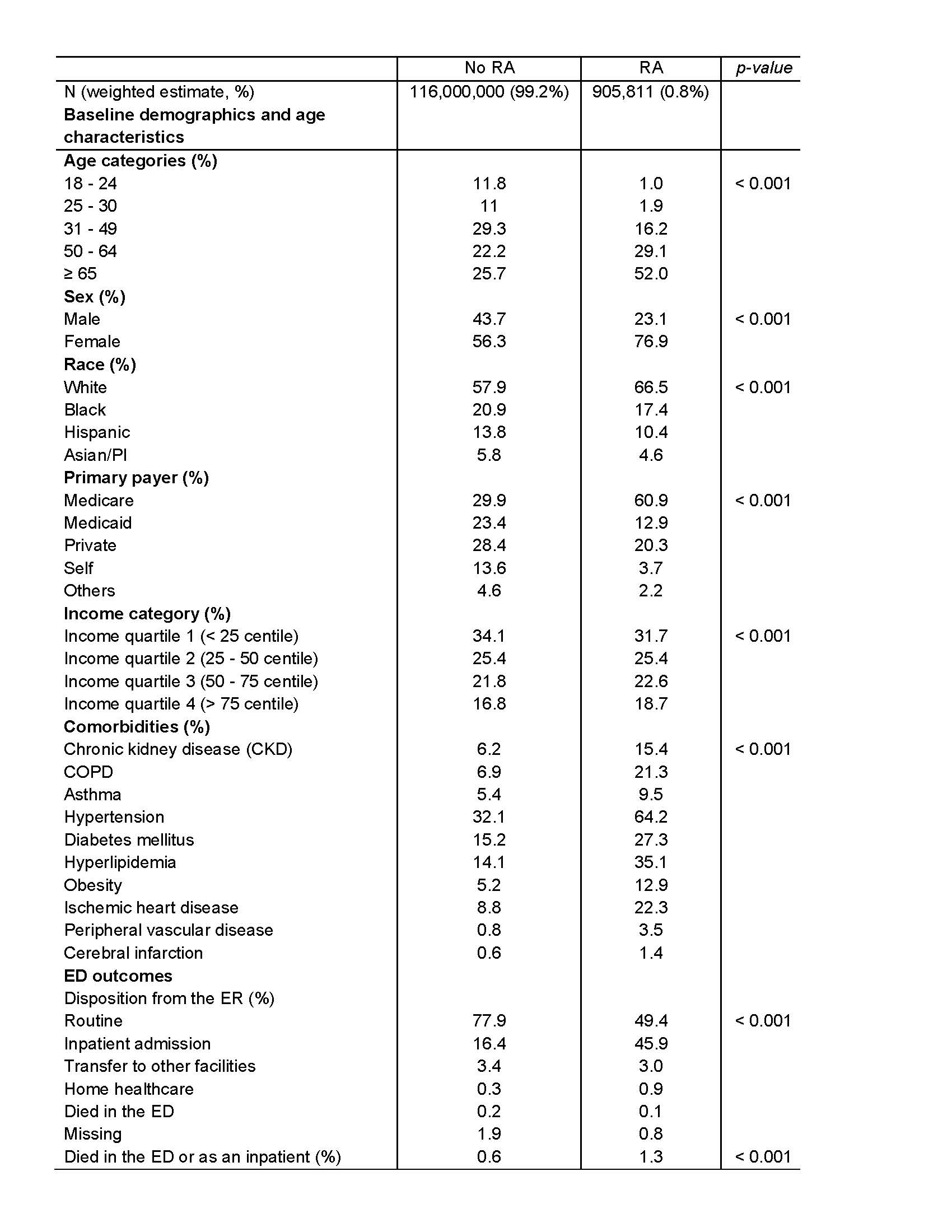
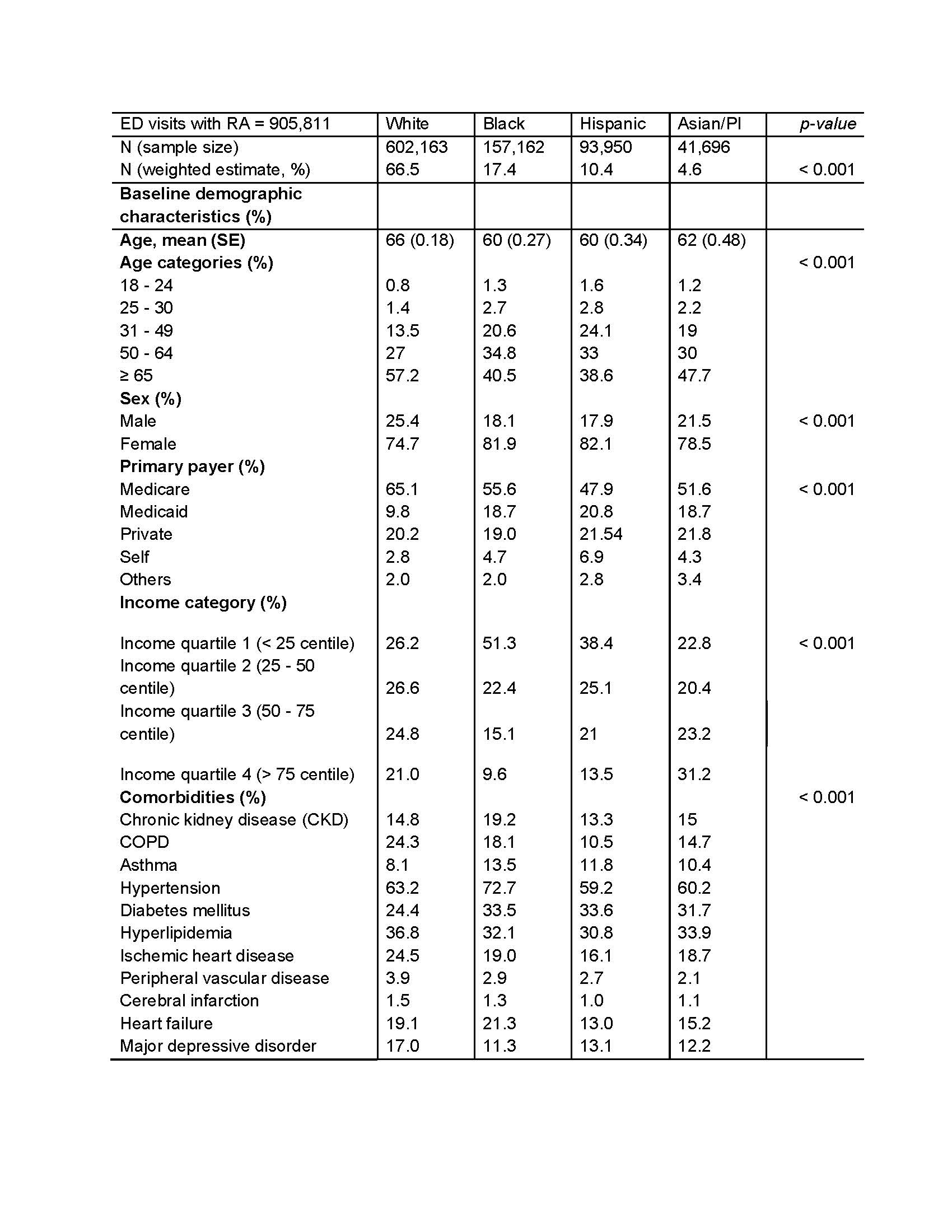
Results: We identified 905,811 (0.8%) ED visits for adults ≥ 18 years with RA. ED visits with RA comprised of a higher proportion of women, White patients, patients aged ≥ 65 years, and those with Medicare as the primary payer, compared to those without RA. Additionally, these patients had a higher comorbidity burden. Compared to 16% of non-RA ED visits, 46% of RA ED visits resulted in inpatient admission (Table 1). A higher proportion of Black and Hispanic RA patients who visited the ED belonged to the younger age categories of 31-49 years (~ 21-24%) and 50-64 years (~ 33-35%) compared to White patients (~ 14 and 27%, respectively). A higher proportion of White patients had Medicare as their primary payer (65% vs 48 – 56% in Non-White patients). More Black and Hispanic RA patients belonged to the lowest income quartile compared to White patients (38-51% vs 26%). Comorbidity patterns varied, with higher proportion of White patient having chronic obstructive pulmonary disease, hyperlipidemia, and ischemic heart disease, while more Black patients had chronic kidney disease, hypertension, and heart failure (Table 2). Increasing age, male sex, and comorbidities were linked to higher odds of inpatient admission. Black race (OR 0.78, p < 0.001), lowest income quartile (OR 0.83, p < .001), and Medicaid coverage (OR 0.86, p < 0.001) were associated with lower odds of inpatient admission (Figure 1). Septicemia was the most prevalent primary ED diagnosis in patients with RA.
Conclusion: RA patients visiting the ED were older, had significantly higher comorbidity burden, and were almost three times more likely to be admitted, compared to non-RA ED visits. Black and Hispanic patients presented at a younger age compared to White patients. Black patients, as well as those with Medicaid coverage, had lower odds of being admitted, indicating potential disparities in admission rates based on racial and other socioeconomic factors. Further clarification of factors influencing need for ED evaluation and hospitalization among RA patients promises to inform preventive care and health equity for this vulnerable population.
To cite this abstract in AMA style:
Bharadiya V, Singh A, Berry P, Feterman Jimenez D, Hughes G, Bays A, Stovall R, Dhital R, Singh N. Burden of Emergency Department Visits and Their Outcomes Among Patients with Rheumatoid Arthritis: Insights from the Nationwide Emergency Department Sample (NEDS) [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/burden-of-emergency-department-visits-and-their-outcomes-among-patients-with-rheumatoid-arthritis-insights-from-the-nationwide-emergency-department-sample-neds/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/burden-of-emergency-department-visits-and-their-outcomes-among-patients-with-rheumatoid-arthritis-insights-from-the-nationwide-emergency-department-sample-neds/