Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Scleroderma renal crisis (SRC) is a major vascular complication of systemic sclerosis (SSc), associated with high morbidity and mortality. Few biomarkers are available to predict SRC and assess its prognosis. SRC and pre-eclampsia share similar clinical phenotype and biological characteristics. The aim of this study was to assess placental growth factor (PlGF), soluble fms tyrosine kinase 1 (sFlt-1) and sFlt1/PlGF ratio as biomarkers in SRC.
Methods: Serum samples from 27 SSc patients with history of SRC (SSc-SRC+) were collected. Biomarker levels were assessed using Cobas Roche® immunoassay and compared to age- and sex-matched SSc patients with no history of SSc (SSc-SRC-) (n = 24), as well as patients with hemolytic uremic syndromes (HUS) (n = 27), malignant hypertension (MHT) (n = 22), and healthy donors with no known vasculopathy (n = 61). The diagnostic performance of the biomarkers was assessed using receiver operating characteristics (ROC) curves, and optimal thresholds determined using Youden’s index. A Cox model analysis was performed to assess the risk of long-term dialysis associated with biomarker elevation.
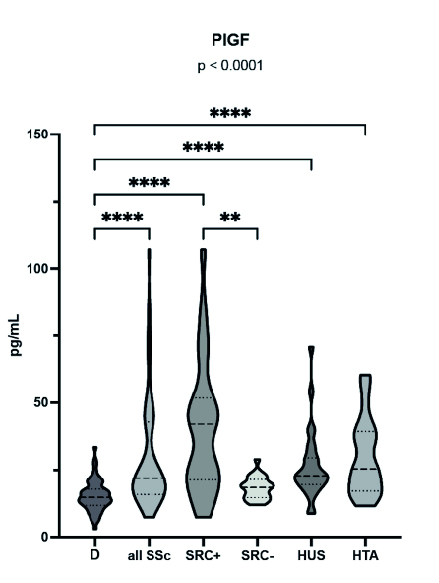
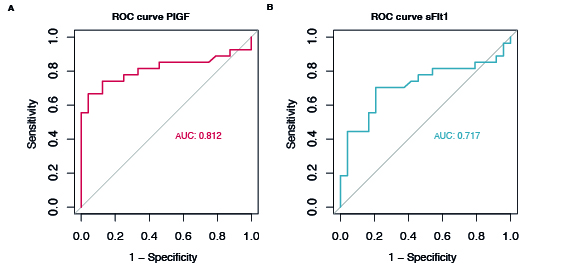
Results: The median [interquartile range] PlGF level (pg/mL) was significantly higher in the serum of SSc-SRC+ patients (42.1 [21.4 – 51.8]) compared to donors (14.7 [11.8 – 17.9]) and SSc-SRC- patients (18.5 [14.7 – 21.5]) (p < 0.0001). PlGF levels were also significantly higher in SSc-SRC+ compared to HUS (22.8 [19.5 – 29.6]) and MHT (25.5 [17.2 – 39.3]) patients (p < 0.0001) (Figure 1). A PlGF level above a threshold of 24.5 pg/mL was associated to an AUC of 81.2% [0.68 – 0.94], with a specificity of 95% and a sensitivity of 67%. sFlt-1, with an AUC of 71% [0.56 – 0.86] and sFlt1/PlGF ratio with an AUC of 67% [0.51 – 0.82] had lower diagnostic performance for the diagnosis of SRC (Figure 2). SSc-SRC+ patients who progressed to end-stage kidney disease had significantly higher levels of PlGF (42.9 [22.4 – 78.2]) compared to patients who did not require long-term dialysis (19.7 [15.6 – 29.7], p = 0.03). PlGF elevation was associated with an increased risk of long-term dialysis with a hazard ratio [CI] of 17.41 [1.88 – 160] (p = 0.012). In contrast to PlGF, sFlt-1 and sFlt-1/PlGF ratio were not significantly associated with an increased risk of long-term dialysis with a hazard ratio of 1 and 0.8 [0.5 – 1.2], respectively.
Conclusion: Serum PlGF accurately identifies the risk of SRC occurrence in SSc patients with a good specificity and may be considered a tool for SRC diagnosis and long-term dialysis risk assessment. These findings suggest that PlGF may serve as a valuable biomarker for SRC diagnosis and prognosis with no additional interest in measuring sFlt-1 and in calculating the sFlt-1/PlGF ratio.
To cite this abstract in AMA style:
Kante A, Legendre P, Joly B, Dunogue b, Hertig A, Terrier B, Massolin E, Ackermann F, Mouthon L, Guibourdenche J, Chaigne B. Diagnostic Performances of Vascular Biomarkers Soluble Fms-like Tyrosine Kinase (sFlt-1) and Placental Growth Factor (PlGF) in Scleroderma Renal Crisis: A Case Control Study [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/diagnostic-performances-of-vascular-biomarkers-soluble-fms-like-tyrosine-kinase-sflt-1-and-placental-growth-factor-plgf-in-scleroderma-renal-crisis-a-case-control-study/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/diagnostic-performances-of-vascular-biomarkers-soluble-fms-like-tyrosine-kinase-sflt-1-and-placental-growth-factor-plgf-in-scleroderma-renal-crisis-a-case-control-study/