Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Although autoimmune myositis (AIM) and interstitial lung disease (ILD) are uncommon in systemic lupus erythematosus (SLE), they are associated with worse outcomes. Myxovirus Resistance Protein 1 (MxA), is a type I interferon-induced GTPase that is sarcoplasm-expressed in muscle biopsies from patients with dermatomyositis and SLE-associated AIM [1]. Autoantibodies against MxA (anti-MxA) are expressed in idiopathic interstitial pneumonia [2]. We assessed the frequency of anti-MxA autoantibodies in SLE patients with AIM and/or ILD, and compared the diagnostic performance of anti-MxA to previously the identified biomarkers for SLE-associated AIM and ILD.
Methods: McGill Lupus Cohort participants (N=551, 2000-2017) without a history of AIM and/or ILD, meeting the 1997 American College of Rheumatology criteria [3], were followed at annual study visits from cohort enrolment until either the date of AIM and/or ILD diagnosis or December 31, 2017. A case-cohort analysis was performed, comparing all patients who developed AIM and/or ILD on follow-up with a randomly selected sub-cohort of SLE patients (N = 72). To determine how anti-MxA compares to previously identified biomarkers in this SLE cohort, we tested for anti-MxA by addressable laser bead immunoassay using full-length human recombinant protein on: 1) baseline samples (first visit starting from January 2000 or enrollment if after this date) and 2) one follow-up sample (randomly selected between baseline and end of follow-up). Follow-up ended at date of AIM and/or ILD diagnosis or death or last date seen or December 31, 2017, whichever came first.
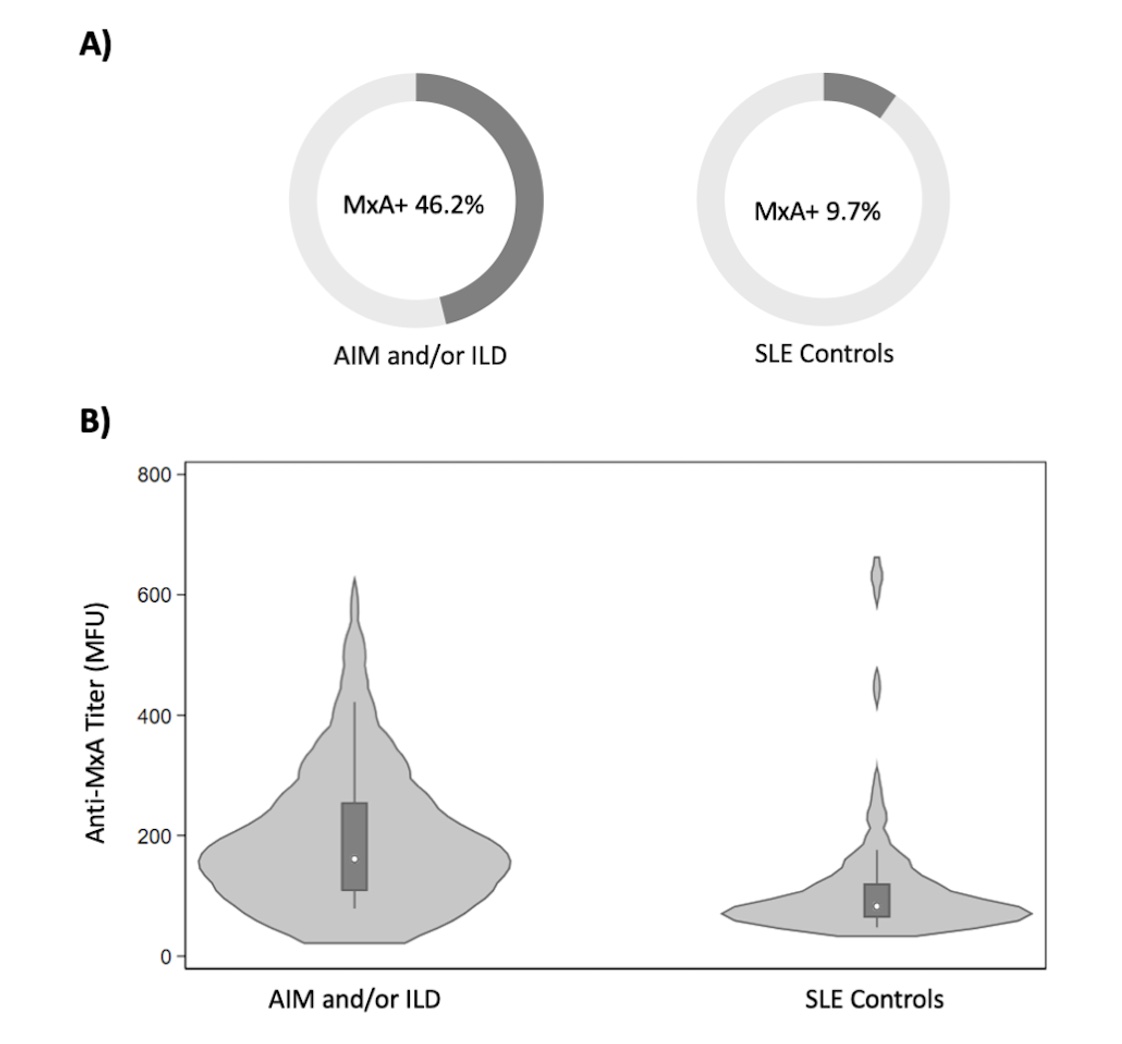
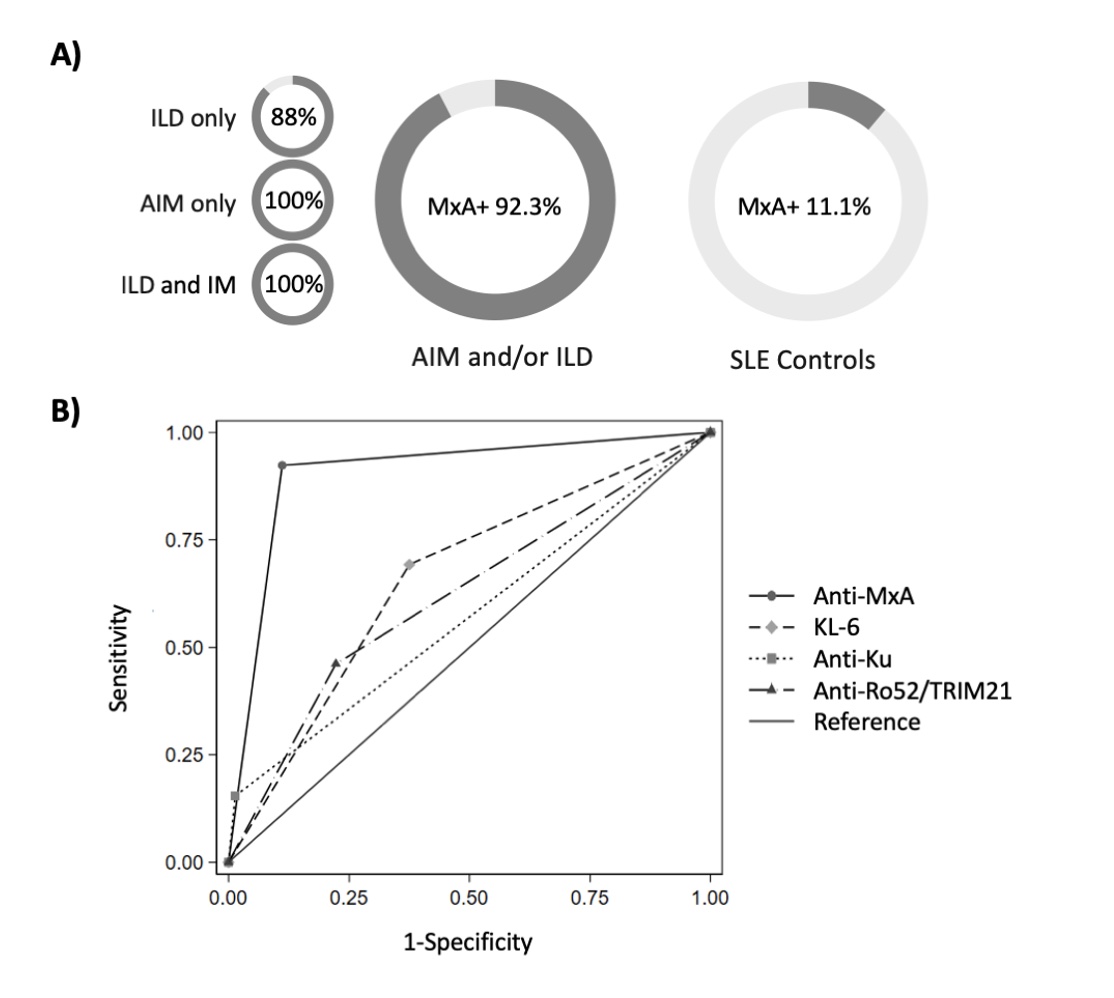
Results: At baseline, there was a greater proportion of anti-MxA positivity among individuals with SLE who later developed AIM and/or ILD compared to those who did not (46.2% vs. 9.7%, respectively) (Figure 1A). Baseline anti-MxA titres were increased in individuals who later developed AIM and/or ILD compared to those who did not (Figure 1B). Considering anti-MxA autoantibodies assessed at baseline and follow-up, almost all AIM and/or ILD cases (12/13, 92.3%) were anti-MxA positive during their disease course (ILD alone 7/8, 87.5%; AIM alone 3/3, 100%; AIM and ILD 2/2, 100%;), while only 11.1% (8/72) of SLE patients without AIM or ILD expressed anti-MxA (Figure 2A). Anti-MxA positivity had high sensitivity (92.3%; 95% CI: 64.0%, 99.8%) and specificity (88.9%; 95% CI: 79.3%, 95.1%) for AIM and/or ILD, with a receiver-operating-characteristic area under the curve (ROC AUC) of 0.91 (95% CI: 0.83, 0.98), which outperformed the ROC AUC for previously identified biomarkers KL-6 (0.63; 95% CI: 0.52, 0.80), anti-Ku (0.57; 95% CI: 0.47, 0.67), and anti-Ro52/TRIM21 (0.62; 95% CI: 0.47,0.77) (Figure 2B).
Conclusion: These results suggest anti-MxA is an important biomarker for AIM and ILD in SLE. Anti-MxA outperformed previously identified biomarkers. A larger study is underway to confirm these findings and examine associations with other SLE features and in other connective tissue diseases.
References:
[1] Xing C, et al., Muscle Nerve. 2024; 69(5): 548-555.
[2] Hamano, Y., et al., Scientific Reports 2017; 7(1): 43201.
[3] Hochberg MC., Arthritis Rheum 1997; 40: 1725.
To cite this abstract in AMA style:
Krustev E, Fritzler M, Bernatsky S, St-Pierre Y, Vinet E, Pineau C, Mendel A, Kalache F, Grenier L, Cotton T, Zahedi O, Choi M. Anti-Myxovirus Resistance Protein 1: A Novel Biomarker for Autoimmune Myositis and Interstitial Lung Disease in Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/anti-myxovirus-resistance-protein-1-a-novel-biomarker-for-autoimmune-myositis-and-interstitial-lung-disease-in-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/anti-myxovirus-resistance-protein-1-a-novel-biomarker-for-autoimmune-myositis-and-interstitial-lung-disease-in-systemic-lupus-erythematosus/