Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Studies of rheumatoid arthritis (RA) have shown that malondialdehyde-acetaldehyde (MAA) protein adducts and anti-MAA immune responses play a pathogenic role in disease progression. Expression of MAA-modified proteins are increased in RA synovium and circulating anti-MAA antibodies are higher in adults with RA than in controls including patients with other rheumatologic conditions.1 Despite marked similarities in disease pathogenesis, the role of MAA and anti-MAA antibodies have not been evaluated in Juvenile Idiopathic Arthritis (JIA). The objective of this study was to compare serum levels of anti-MAA antibody in patients with JIA to levels in controls and to identify any potential factors in JIA associated with anti-MAA expression. We tested the hypothesis that anti-MAA antibodies would be higher in JIA and, among those with JIA, highest in children with polyarticular disease as well as those who are CCP or RF positive.
Methods: Serum samples were obtained from children diagnosed with all subtypes of JIA (except for systemic JIA) from a single pediatric medical center. Serum IgM, IgG, and IgA anti-MAA antibodies were measured by ELISA. Through chart review, demographic information as well as ANA, RF, CCP, and HLA-B27 status was determined. In initial analyses, anti-MAA antibody concentrations were compared with values measured in a cohort of unmatched healthy controls without JIA using a Student’s t-test. Anti-MAA antibody levels were compared across six JIA subtypes using Kruskal-Wallis tests. We further compared patients’ characteristics and anti-MAA antibody levels between those with positive and negative biomarkers using chi-square or Fisher’s exact tests for categorical variables and Wilcoxon rank-sum tests for continuous variables. Analyses were performed in Stata MP Release 18.2
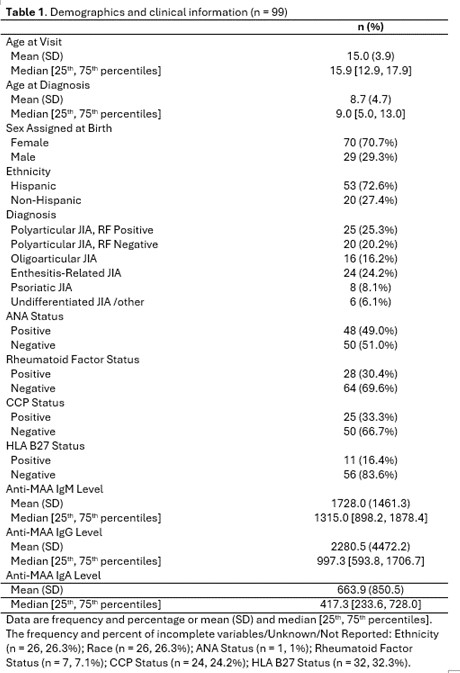
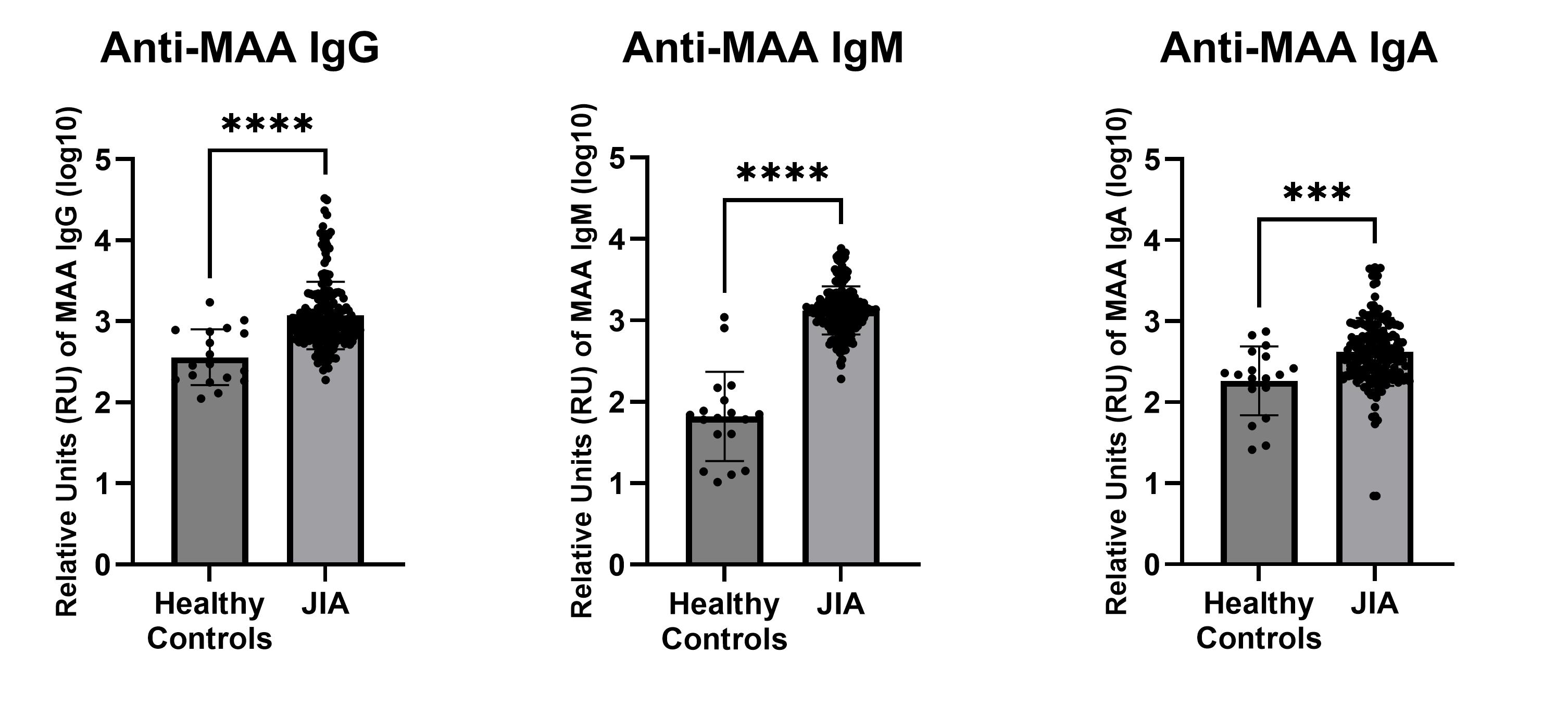
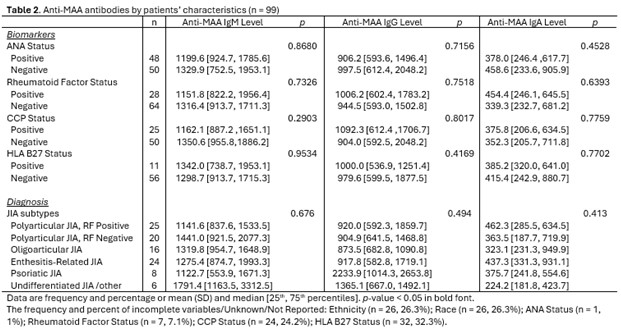
Results: We studied 99 JIA participants with a mean age at visit of 15 years, mean age at JIA diagnosis of 8.7 years, 72.6% Hispanic, 70.7% female, 49% ANA positive, 30.4% RF positive, 33.3% CCP positive, and 16.4% HLA-B27 positive (Table 1). IgM, IgG and IgA anti-MAA antibody levels were higher in JIA patients (n=99) compared to previously obtained group of unmatched, healthy controls (n=18; p≤0.0014) (Figure 1). Among those with JIA, there were no significant differences in levels of anti-MAA antibodies by arthritis subtype, ANA, RF, CCP or HLA-B27 status (Table 2).
Conclusion: This study showed that humoral immunity to MAA is increased in the context of JIA, with similar levels of expression observed across JIA subtypes and by other biomarkers commonly assessed in JIA. These results support further research using large patient samples to determine diagnostic as well as prognostic value of anti-MAA antibodies in JIA. Significant findings could further open the door for additional MAA studies in the realm of pediatrics, as it has also been shown to be positive in other autoimmune conditions such as pediatric IBD and lupus in adults.
To cite this abstract in AMA style:
Thiele G, Hayati Rezvan P, Cidon M, Hunter C, Duryee M, Mikuls T, Thiele G. Evaluation for the Presence of Antibodies to Malondialdehyde-Acetaldehyde Adduct in Juvenile Idiopathic Arthritis and Its Subtypes [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/evaluation-for-the-presence-of-antibodies-to-malondialdehyde-acetaldehyde-adduct-in-juvenile-idiopathic-arthritis-and-its-subtypes/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/evaluation-for-the-presence-of-antibodies-to-malondialdehyde-acetaldehyde-adduct-in-juvenile-idiopathic-arthritis-and-its-subtypes/