Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Interstitial lung disease (ILD) is a common complication of connective tissue diseases (CTDs), significantly influencing prognosis and mortality. The prevalence and characteristics of new diagnoses of connective tissue disease (NDC) that present with ILD as the first symptom are not well studied, despite their influence on treatment. The purpose of this study is to investigate the prevalence of NDC in a cohort during their 1st visit to a specific multidisciplinary ILD unit and to describe the clinical, serological, and radiological characteristics of subgroups of patients with final diagnoses of NDC, ILD with autoimmune positivity (ILD-AI), interstitial pneumonia with autoimmune features (IPAF), and non-autoimmune ILD (NA-ILD).
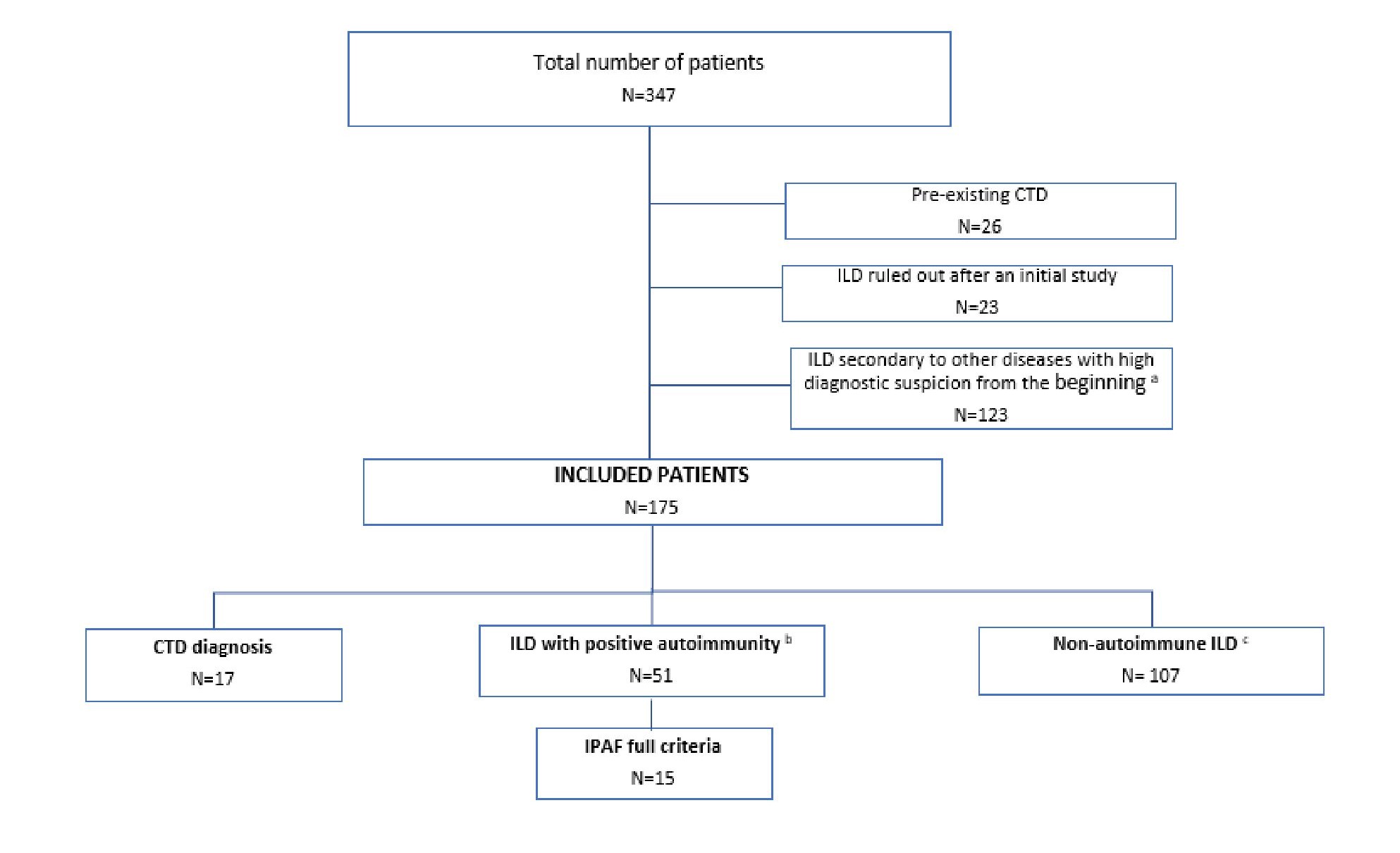
Methods: Retrospective study based on all the first visits referred to a specialized pulmonology ILD clinic (Jan 2021-Oct 2023). 347 medical records were reviewed, with a final sample of 175 (Fig. 1).
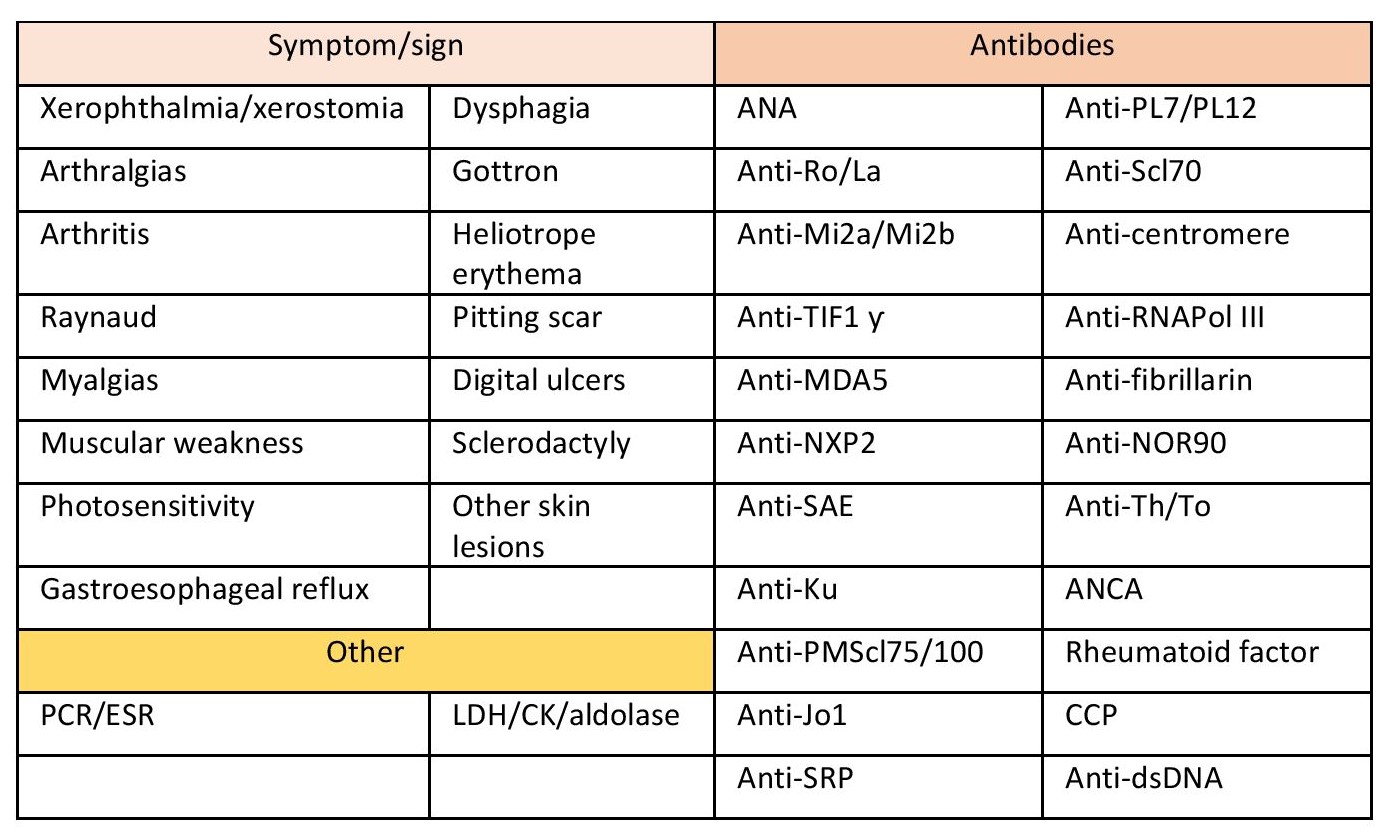
Those visits were standardized to optimize the diagnosis of potential CTD associated with ILD. All patients underwent a high-resolution CT and standardized clinical and serological assessments (Fig. 2).
Upon suspicion of NDC, a rheumatological evaluation was conducted using the ACR/EULAR classification criteria for final diagnoses. Descriptive and univariate analyses were performed between the groups (NDC, ILD-AI, IPAF, and NA-ILD) using the Chi-square test/Fisher’s exact test for categorical variables and the ANOVA test for quantitative ones.
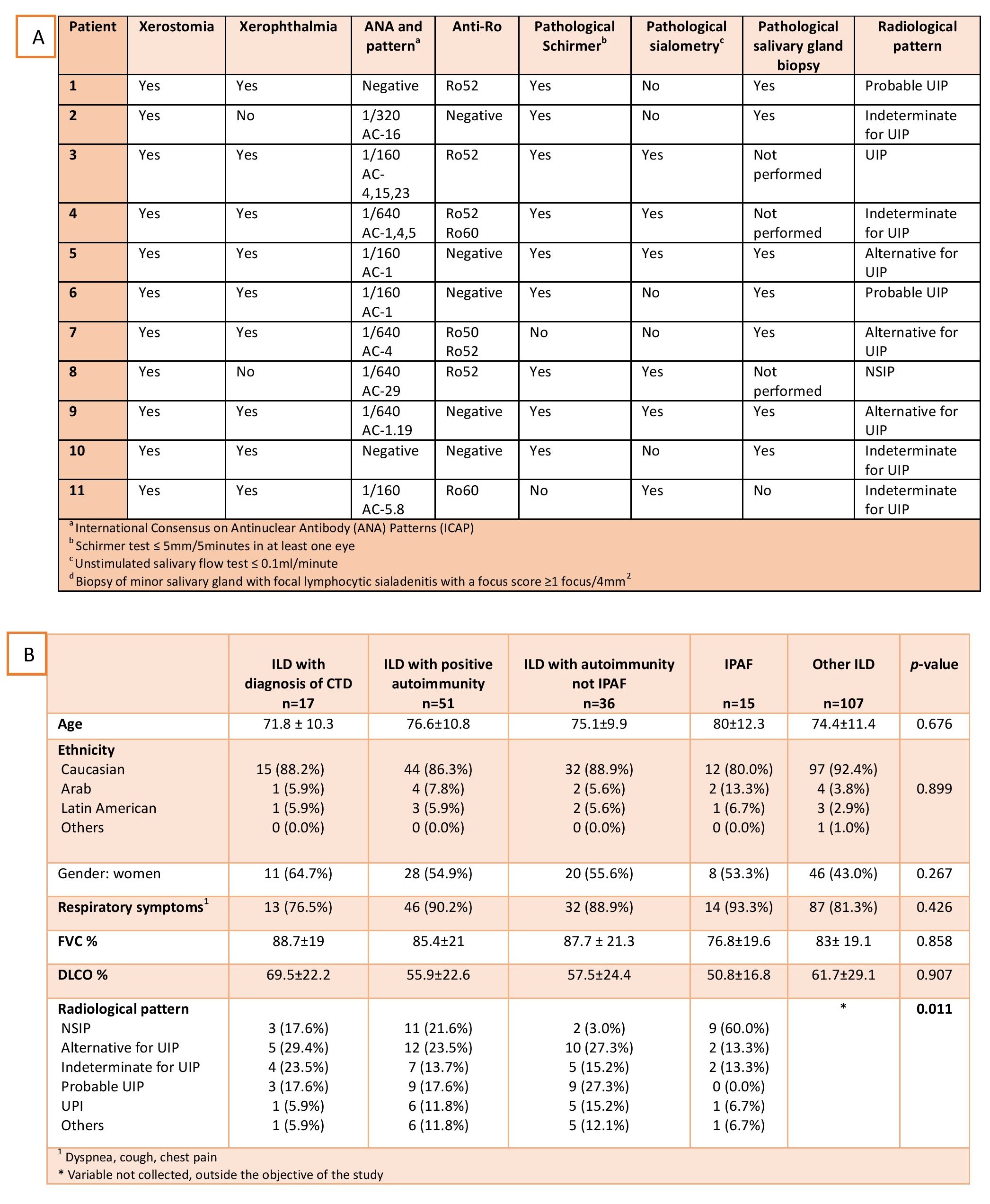
Results: The prevalence of NDC and ILD-AI were 9.71% (17/175) and 29.14% (51/175). Primary Sjögren’s syndrome (pSS) was the most common CTD, accounting for 64.7% (11/17), being anti-Ro/anti-La seronegative in 45.5% (5/11) and with histological criteria crucial for diagnosis in 54.4% (6/11). Other diagnosed CTD were rheumatoid arthritis (2/17), systemic sclerosis (1/17), and immune-mediated myopathies (3/17).
Among the 51 ILD-AI cases, the most common serological criterion was ANA≥320 (45.1%, 23/51), and the most prevalent specific autoantibody (aa) anti-PL7 (13.72%, 7/51). Within the ILD-AI group, 29.4% (15/51) met criteria for IPAF, with the most frequent serological criterion being ANA≥320 (53.3%, 8/15), regardless of pattern and specificity, without any predominant aa. Among the ILD-AI group, 3 patients were diagnosed with ANCA-associated ILD (all anti-MPO).
The radiological alternative pattern for Usual Interstitial Pneumonia (UIP) was the most prevalent in the NDC (29.4%) but 23.52% presented with a probable UIP/UIP pattern. The Nonspecific Interstitial Pneumonia (NSIP) pattern was the most prevalent in the IPAF subgroup (60%). (Tab A/B).
Conclusion: pSS was the most frequent CTD initially presenting as ILD, accounting for 64.7% of the NDC cases. Minor salivary gland biopsy enabled diagnosis in more than half of the cases, highlighting its importance, especially in seronegative patients (up to 45.5%) with sicca syndrome.
We consider the concept of ILD-AI to be particularly relevant, as a significant percentage of patients presented with the UIP/probable UIP ILD type, which is not included in the IPAF criteria so they could not be diagnosed despite meeting IPAF serological criteria.
a. Sarcoidosis, Langerhans cell histiocytosis, eosinophilic pneumonia, post-infectious organizing pneumonia.
b. This group includes interstitial lung diseases (ILDs) with positive autoimmunity (using the serological criterion os Interstitial Pneumonia with Autoimmune Features IPAF) but that do not meet criteria to establish a definitive connective tissue disease or IPAF in the strict sense.
c. Smoking-related interstitial pneumonia, hypersensitivity pneumonitis, drug toxicity, idiopathic pulmonary fibrosis, unclassified.
B. Characteristics of the patients studied. ILD: Interstitial lung disease; CTD: Connective Tissue Diseases; IPAF: interstitial pneumonia with autoimmune features; FVC: predicted forced vital capacity (%); DLco; diffusing capacity of the lungs for carbon monoxide; NINE: non-specific interstitial pneumonia; UIN: usual interstitial pneumonia
To cite this abstract in AMA style:
Meraz-Ostiz J, Puiggròs-Ferrer A, Bou N, Carrión-Barberà I, Monfort J, Pérez-García C, Badenes D, Balcells E, Pros-Simon A. Interstitial Lung Disease as the First Clinical Manifestation of Connective Tissue Diseases [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/interstitial-lung-disease-as-the-first-clinical-manifestation-of-connective-tissue-diseases/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/interstitial-lung-disease-as-the-first-clinical-manifestation-of-connective-tissue-diseases/