Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: The connection between airway inflammation as seen in patients with asthma and rheumatoid arthritis (RA) has been suggested by previous epidemiologic studies. For instance, asthma and chronic obstructive pulmonary disease have been associated with increased prevalence of RA in prospective, longitudinal studies when compared to healthy controls. RA-associated autoantibodies, including antibodies to citrullinated peptides (ACPA) have been found to be significantly higher in populations of patients with lung diseases such as pulmonary fibrosis than seen in healthy controls. The purpose of our study is to evaluate the association between asthma and serum ACPA antibodies when compared to healthy controls in two large, well characterized asthma cohorts.
Methods: Our study leveraged two large asthma cohorts that were collected prospectively for research efforts at 8 tertiary care centers in the United States. Our patient population included 189 patients from a large multi-center prospective asthma study and 166 patients in our validation cohort of asthma patients collected a single medical center and 94 healthy controls collected from a local health fair screening sample. Both asthma cohorts included patients with mild, moderate and severe asthma based on international guidelines. Levels of serum ACPA IgG and IgA isotypes were measured via ELISA using kits supplied by Inova Diagnostics, Inc., San Diego, CA. Comparisons of ACPA titers across cohorts were performed using Wilcoxon rank sum test with continuity correction. ACPA positivity was determined based on 3 standard deviations above the mean in healthy controls. ACPA positivity proportion comparisons were made via Pearson’s Chi-squared test with Yate’s continuity correction.
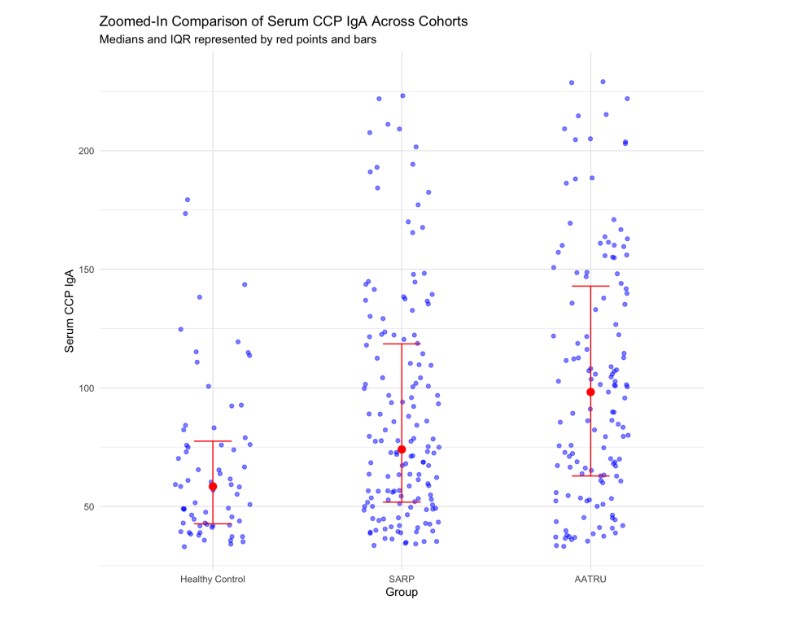
Results: The median ACPA IgA in the discovery asthma cohort was 74.9 u/mL (IQR: 90.1) and 103.0 u/mL (IQR: 99.4) in the validation asthma cohort, while the healthy control median was 49.0 u/mL (IQR: 37.7). ACPA IgA titers were significantly higher in both the asthma discovery and validation cohorts than in the healthy control group (p-values for both comparisons: < 0.001) (Figure 1). In terms of proportion of ACPA positivity, the discovery asthma and validation asthma cohorts had 37.3% and 22.2% ACPA IgA positivity compared to 3.7% in the control cohort which were both significantly greater proportion than controls (p-value < 0.001 for both). There was no significant difference found in ACPA IgG across these comparisons.
Conclusion: We observed that patients with asthma had significantly higher IgA ACPA titer and IgA ACPA positivity when compared to healthy controls in a discovery and validation cohort. This suggests a potential relationship between airway inflammation such as that seen in patients with asthma and development of serum ACPA (IgA). This finding supports the role of the lung mucosa as a site for ACPA development.
To cite this abstract in AMA style:
Rorah D, Ngo L, Matson S. Asthma Is Associated with Increased Serum IgA Antibodies to Citrullinated Peptide Antigenscompared to Healthy Controlsin Discovery and Validation Cohorts [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/asthma-is-associated-with-increased-serum-iga-antibodies-to-citrullinated-peptide-antigenscompared-to-healthy-controlsin-discovery-and-validation-cohorts/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/asthma-is-associated-with-increased-serum-iga-antibodies-to-citrullinated-peptide-antigenscompared-to-healthy-controlsin-discovery-and-validation-cohorts/