Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Activated fibroblast-like synoviocytes (FLS) are important mediators of synovitis and structural damage in rheumatoid arthritis (RA)[1]. Granulocyte-macrophage colony-stimulating factor (GM-CSF, encoded by the CSF2 gene) is released from activated RA-FLS and promotes the production of pro-inflammatory cytokines from macrophages, which in turn activates FLS creating a viscous cycle[2]. We investigated the effects of anti-rheumatic drugs on gene expression, in particular RA risk genes such as CSF2, in activated RA-FLS, and on cytokine release from RA synoviocyte cultures.
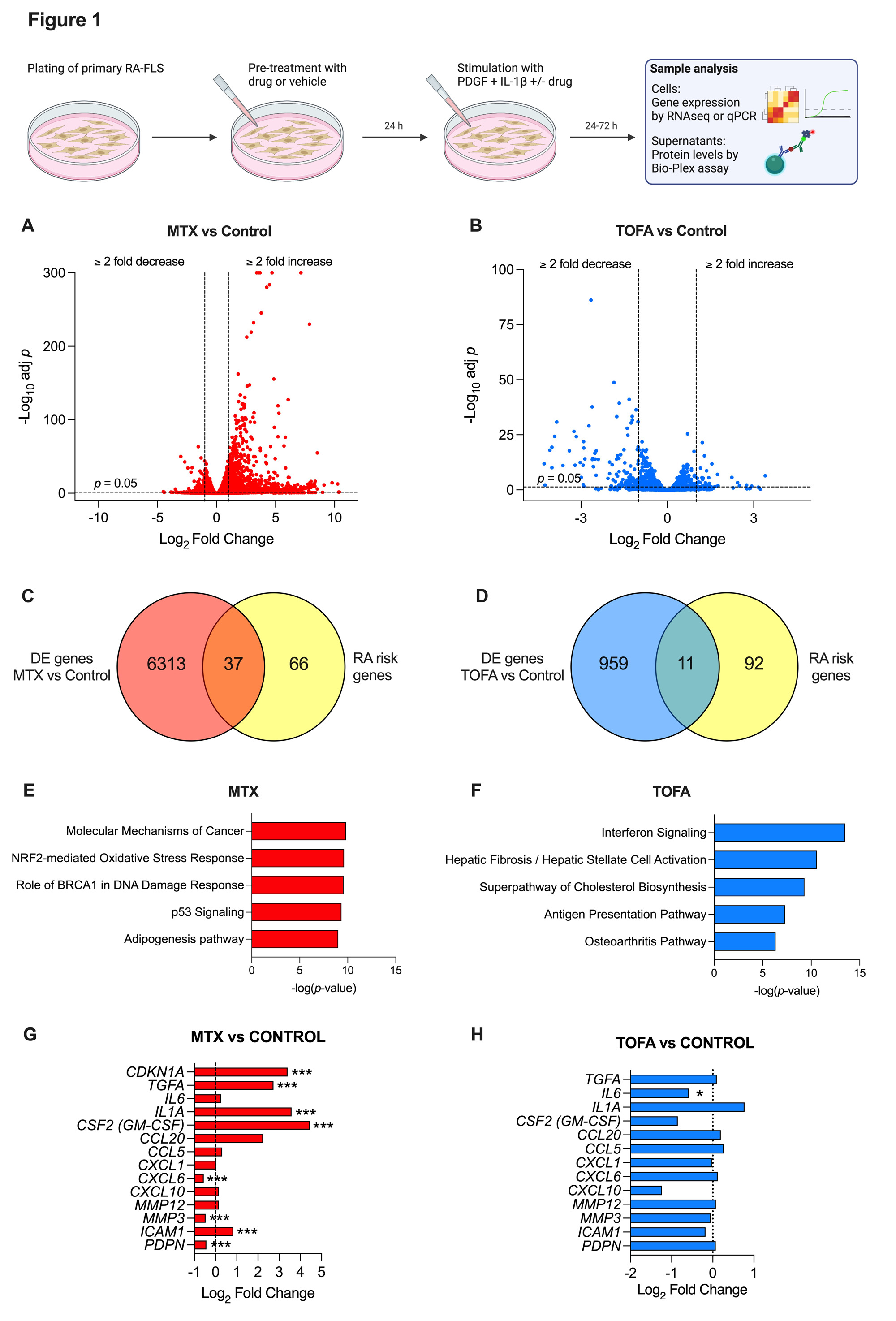
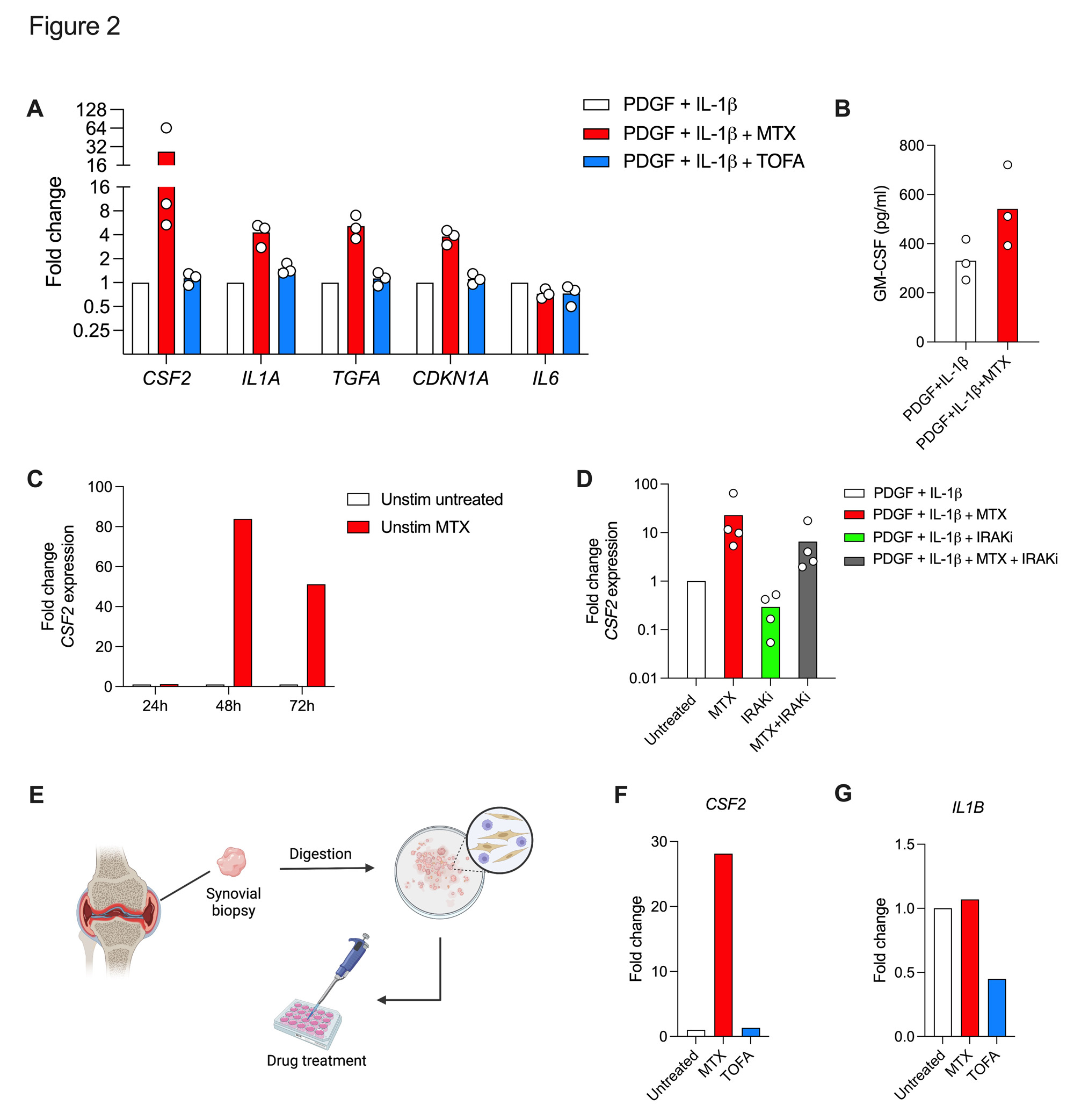
Methods: Primary FLS were established from synovial tissue collected from patients with RA undergoing arthroplasty or synovial biopsy. FLS were pre-treated with methotrexate (MTX), tofacitinib (TOFA, janus kinase inhibitor), zimlovisertib (IRAK4 inhibitor) or vehicle followed by stimulation with platelet-derived growth factor (PDGF) and interleukin-1β (IL-1β) for 24-72 hours (Fig.1, top). An RA ex-vivo synovial bioassay was performed according to Kuo et al.[3]. Cells were collected for RNAseq or qPCR, and supernatants were analyzed for protein concentrations using Bio-Plex assay.
Results: MTX demonstrated an overall activation of gene expression in PDGF+IL-1β stimulated RA-FLS compared to untreated (6350 differentially expressed (DE) genes), and to TOFA treated (970 DE genes) samples (Fig. 1A-B). MTX had a greater effect on RA risk genes (35 % DE in MTX vs CON) compared to TOFA (10 % DE in TOFA vs CON) (Fig.1C-D). Pathway analysis showed largest effects on Molecular mechanisms of cancer (MTX) and Interferon signaling (TOFA) respectively (Fig. 1E-F). Targeted analysis revealed that MTX in addition to the known induction of CDKN1A (p21)[4], profoundly increased CSF2, IL1A and TGFA expression compared to control treated activated FLS (Fig.1G). TOFA reduced IL6 and CXCL10 expression as expected (Fig.1H). RNAseq data were confirmed by qPCR and on protein level in FLS supernatants (Fig.2A-B). Furthermore, MTX induced CSF2 expression also in unstimulated RA-FLS (Fig.2C). IRAK4i could not prevent the increased GM-CSF expression by MTX in stimulated RA-FLS (Fig.2D). MTX induced CSF2 expression in RA ex-vivo synovial cultures (Fig. 2E-F) and failed to reduce IL-1β expression as opposed to TOFA (Fig.2G).
Conclusion: Methotrexate treatment augments the release of GM-CSF from RA-FLS and leads to sustained cytokine production from synoviocytes. This off-target effect might contribute to the persistence of synovitis.
To cite this abstract in AMA style:
Bergström B, Selldén T, Bollmann M, Svensson M, Hultgård Ekwall A. Methotrexate Augments the Release of Granulocyte-macrophage Colony-stimulating Factor from Activated Rheumatoid Arthritis Fibroblast-like Synoviocytes – Possible Consequences for Persistence of Joint Inflammation [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/methotrexate-augments-the-release-of-granulocyte-macrophage-colony-stimulating-factor-from-activated-rheumatoid-arthritis-fibroblast-like-synoviocytes-possible-consequences-for-persistence-of-joint/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/methotrexate-augments-the-release-of-granulocyte-macrophage-colony-stimulating-factor-from-activated-rheumatoid-arthritis-fibroblast-like-synoviocytes-possible-consequences-for-persistence-of-joint/