Session Information
Date: Monday, November 13, 2023
Title: (1221–1255) Pediatric Rheumatology – Clinical Poster II: Connective Tissue Disease
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Juvenile dermatomyositis (JDM) is an idiopathic inflammatory myopathy that causes muscle weakness, rash, vascular changes, or other organ involvement. The phenotypes may vary, and studies suggest a correlation between myositis-specific antibodies (MSA), clinical presentation, and course. This is thought to be due to specific cytokine profiles activated by these antibodies. Melanoma Differentiation-Associated Protein-5 (MDA5) is an MSA associated with clinically amyopathic dermatomyositis and lung disease with high risk for rapidly progressive interstitial lung disease. This study aims to highlight the clinical manifestations of MDA5+ JDM and disease course in a racially and ethnically diverse population. We also aim to assess racial disparities in time-to-diagnosis from cutaneous symptom onset.
Methods: After Institutional Review Board approval was obtained, we conducted a retrospective chart review of patients diagnosed with MDA5-positive JDM at Texas Children’s Hospital.Clinical characteristics at the time of diagnosis, 6-month, 12-month, and most recent visits were recorded.
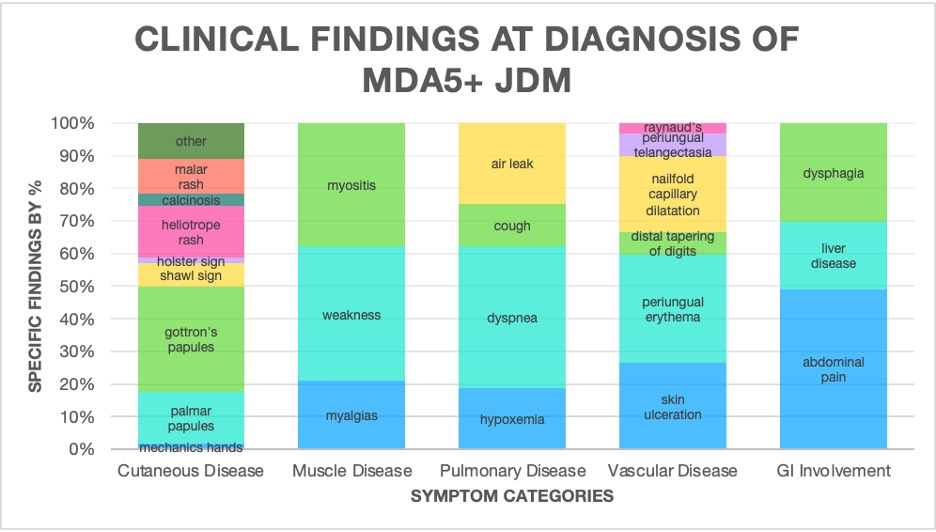
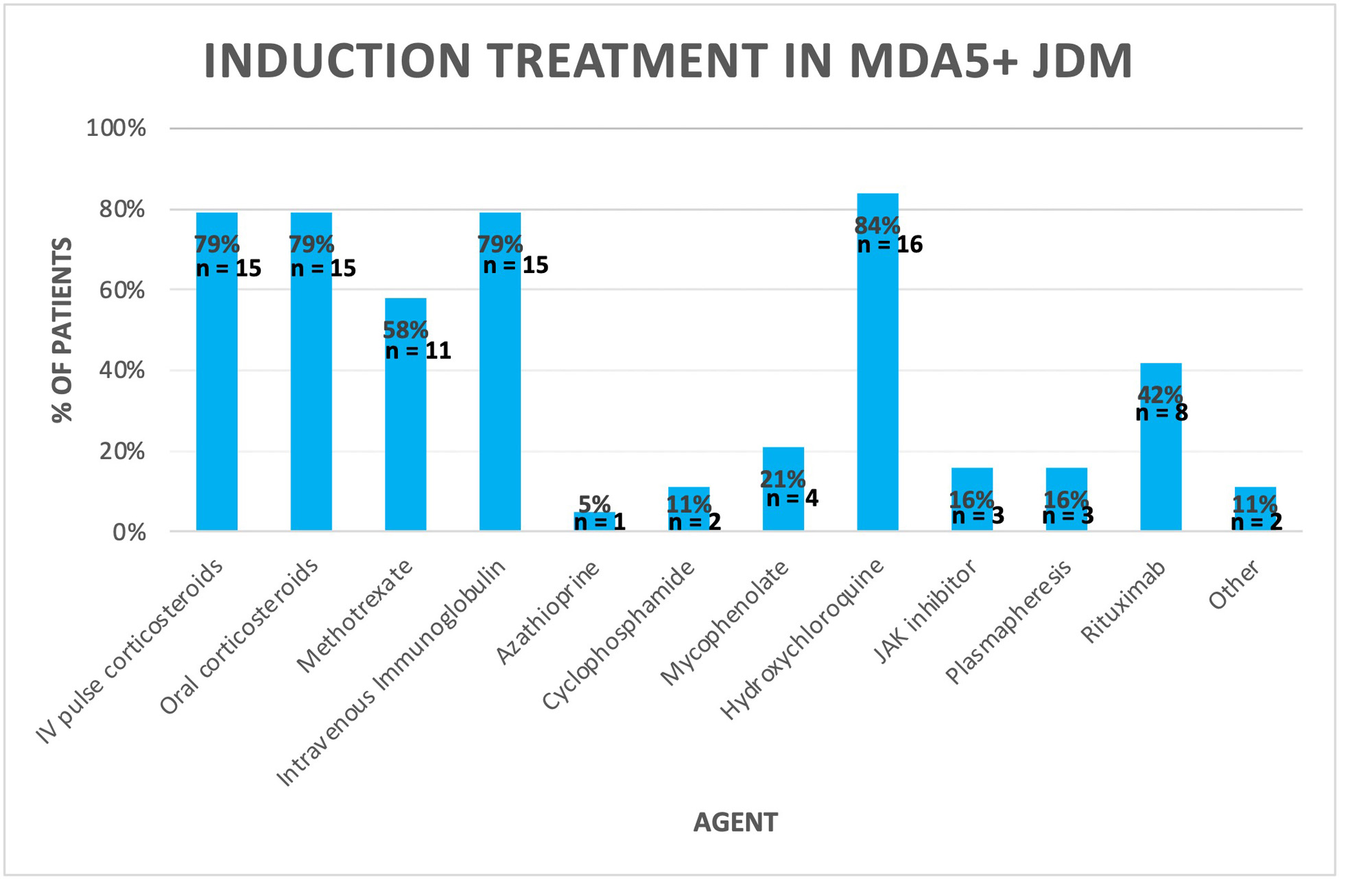
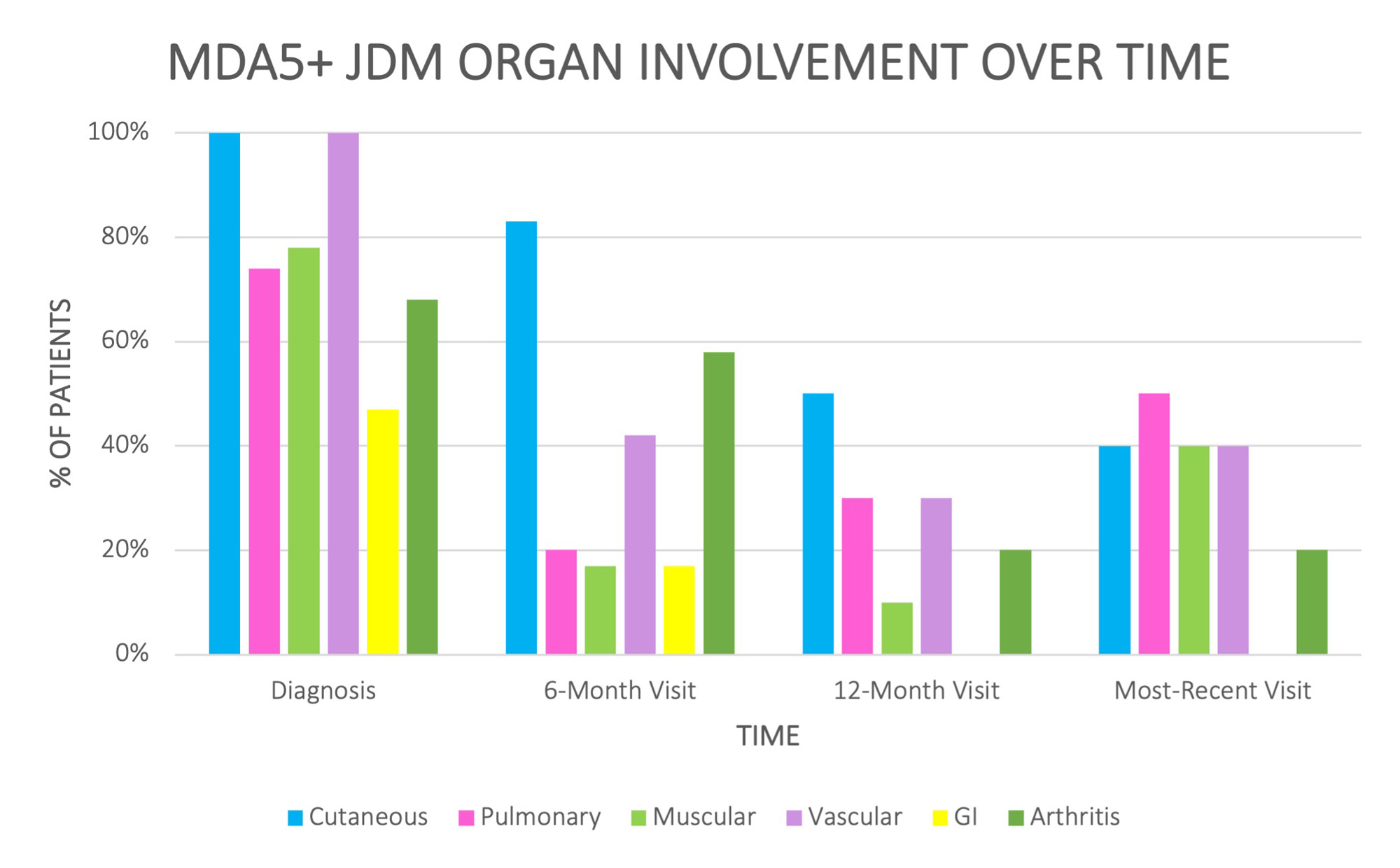
Results: Nineteen patients were included, with a mean age of 9.9 years (range 3-18), 68% female, 21% Black, 79% White, and 68% Hispanic. Figure 1 shows the clinical findings at presentation. All had cutaneous and vascular features, 78% had muscle disease, 74% had interstitial lung disease, and 47% had gastrointestinal (GI) symptoms. Most common skin findings were Gottron’s papules (95%), palmar papules (47%), and heliotrope rash (47%). Median time in months from onset of cutaneous symptoms to diagnosis was 5.5 among Black patients, 5 among Hispanic, and 3 among White Non-Hispanic. Three patients had a lung biopsy, with the most common findings of organizing pneumonia and diffuse alveolar damage. Figure 2 summarizes induction treatment given. 8% of patients had clinical remission at 6-month follow-up, 30% at 12 months, and 50% at last visit (mean of 31.1 months, range: 6-70).Two patients diagnosed at age 3 years had progressive, diffuse alveolar damage resulting in death shortly after diagnosis. At last follow up, 20% still required corticosteroids, 30% required intravenous immunoglobulin (IVIG), and 20% required rituximab. While arthritis, cutaneous symptoms, and GI symptoms improved over time, vascular, muscular, and lung disease were persistent at last visit (Figure 3).
Conclusion: MDA5+ JDM patients in this cohort presented with prominent cutaneous and vascular disease. Lung disease was present early and persisted late in disease course. Half of patients had not reached remission at the last visit, and several continued to require steroids, IVIG, and B-cell depletion. Further studies comparing these patients to non-MDA5 controls may help characterize the role of MDA5 in these findings. While this study does not show a significant difference in time to diagnosis from onset of cutaneous symptoms between racial and ethnic groups, the sample sizes were small. More data on time to diagnosis, especially in Black and Hispanic patients, is needed to assess for delays in diagnosis, as there continues to be a need for education and recognition of cutaneous features in dark skin tones.
To cite this abstract in AMA style:
Gist D, Molina S, Pereira M, Ramirez A, Yildirim-Toruner C, De Guzman M. Melanoma Differentiation-Associated Protein-5 in Juvenile Dermatomyositis: A Single Center Cohort [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/melanoma-differentiation-associated-protein-5-in-juvenile-dermatomyositis-a-single-center-cohort/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/melanoma-differentiation-associated-protein-5-in-juvenile-dermatomyositis-a-single-center-cohort/