Session Information
Date: Monday, November 13, 2023
Title: (1221–1255) Pediatric Rheumatology – Clinical Poster II: Connective Tissue Disease
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: JDM is a rare vasculopathy of unknown etiology characterized by typical rashes and proximal weakness. JDM has been associated with gingivitis, which can be triggered by microbial dysbiosis and has been implicated in the etiology of systemic autoimmune disease. This study aimed to characterize the relationship between oral inflammation and vasculopathy with JDM disease activity.
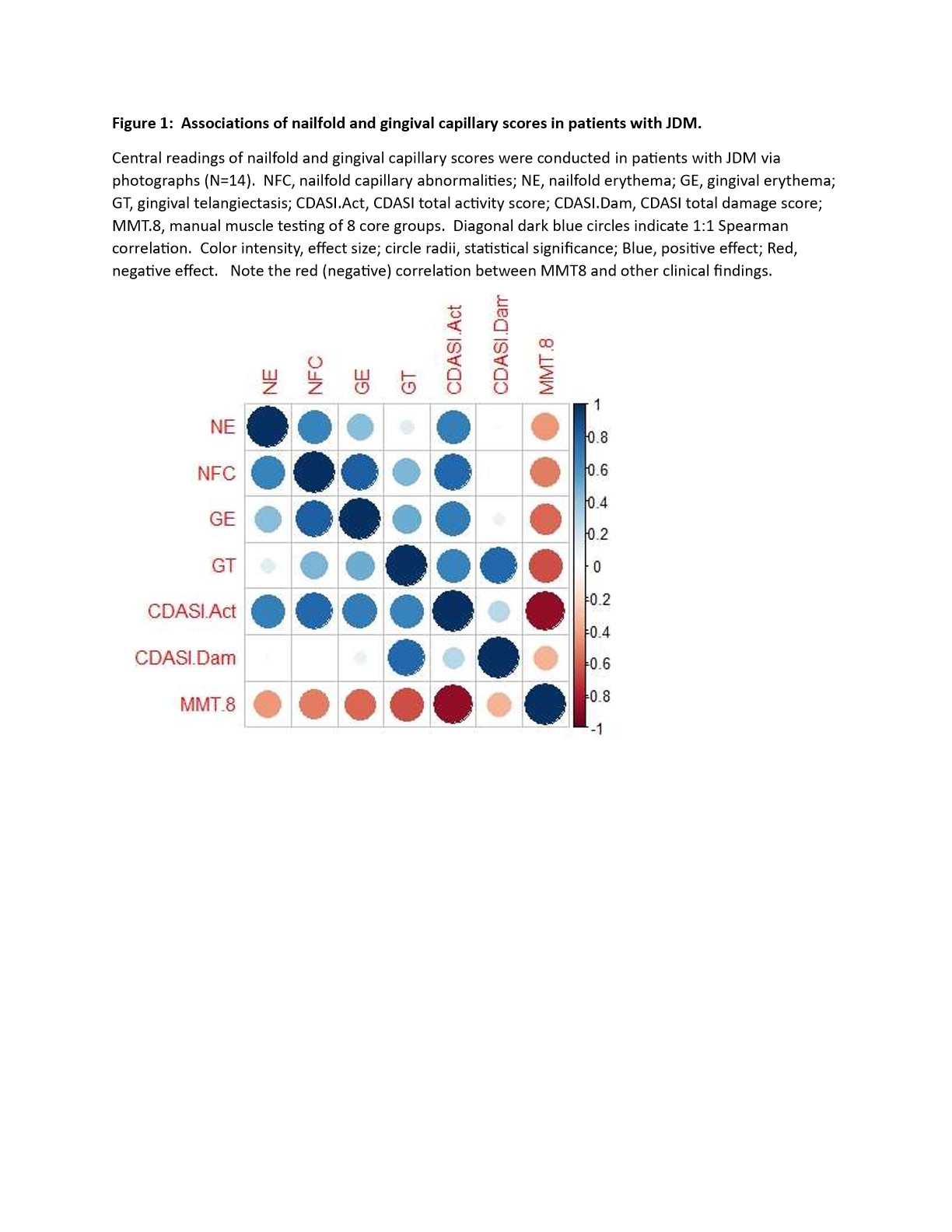
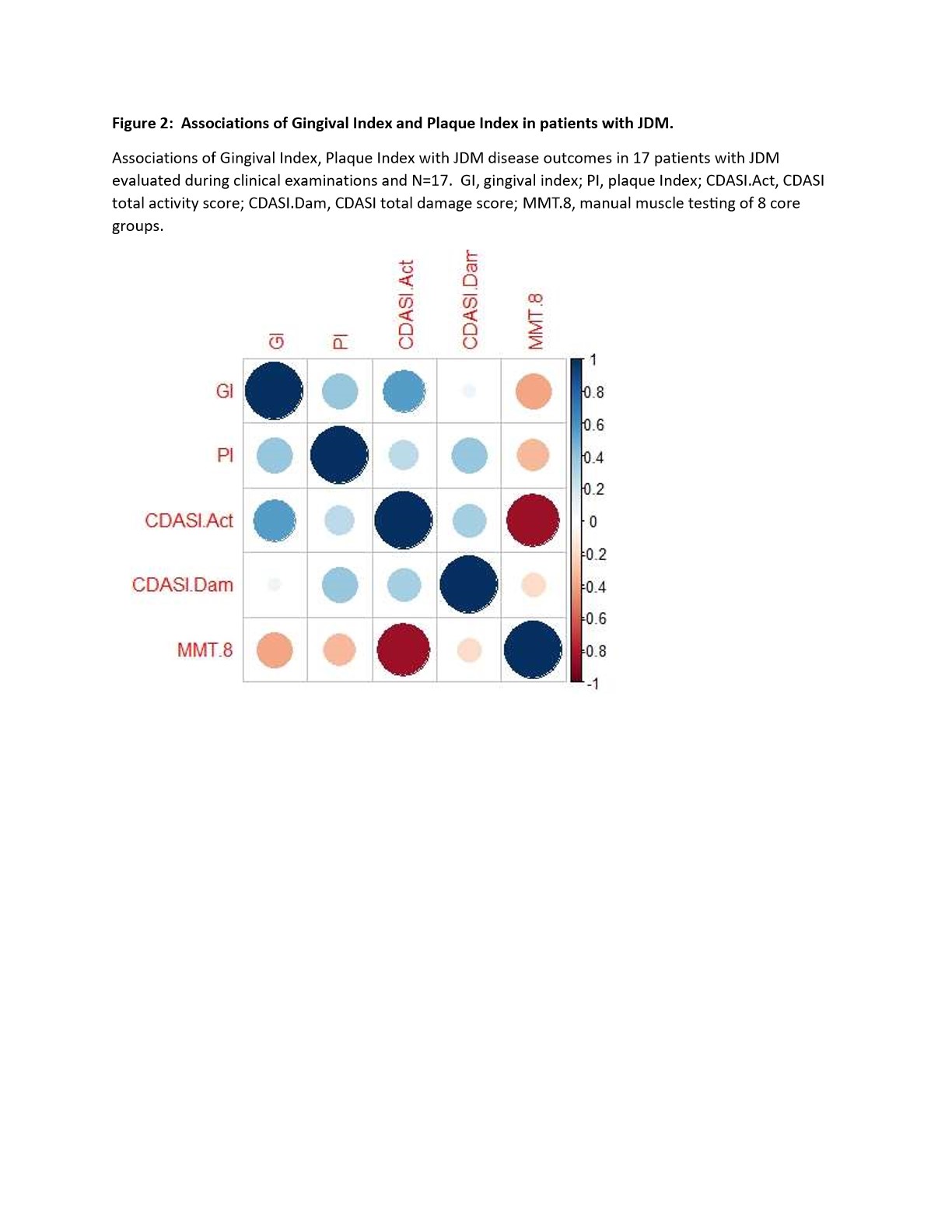
Methods: A prospective pilot observational study was conducted at two centers. Patients met probable or definite Bohan and Peter criteria for JDM, and were excluded for co-existing autoimmune diagnoses, antibiotics within 3 months of enrollment, or gingival erythema secondary to tooth eruption or orthodontic appliances. Gingival erythema, telangiectasias, gingival index, and plaque index were scored by dentists and dental hygienists. Myositis disease activity measures such as manual muscle testing of 8 core groups (MMT8), Cutaneous DM Disease Area and Severity Index (CDASI), and nailfold capillaroscopy (NFC) were assessed by pediatric rheumatologists. To conduct parallel evaluations of vasculopathy in nailfolds and gingiva, we developed a central dichotomous scoring system averaging the presence or absence of erythema and telangiectasias from photographs over 6 anterior teeth and 10 fingers. With uncertain distribution and variance patterns in JDM, we elected to use Spearman’s correlation despite small sample size.
Results: Seventeen subjects ages 3.8-15.5 (mean 8.9) years, with 9 females were included. The mean MMT8 was 140; eleven met PRINTO criteria for clinically inactive disease. The mean CDASI activity score was 6.5 and mean CDASI damage score 1.8.In evaluation of photographs, reliability was good: with Cohen’s Kappa k=0.860 and 0.940 for NFC telangiectasia and erythema and k=0.840 and 0.814 for gingival telangiectasias and erythema. Excellent correlation was found between gingival erythema and presence of NFC abnormalities (r=0.85, p=0.003) and between the presence of gingival telangiectasias and CDASI Damage (r=0.74, p=0.009), with moderate correlation between gingival erythema and MMT8 (r=-0.36, p=0.012) (Figure 1).There was a moderate correlation between Gingival Index and CDASI Activity (r=-0.56, P=0.02) (Figure 2).
Conclusion: We systematically quantified gingival and NFC vasculopathy in JDM and found correlations between signs of oral vasculopathy and both skin and muscle disease, suggesting related pathogenic processes. Future mechanistic studies are needed to elucidate mechanisms, including whether gingival vasculopathy remains an underrecognized primary vasculopathic manifestation of JDM.
To cite this abstract in AMA style:
Chow A, Song H, Brenchley L, Bayat N, Eckert M, Koester S, Schiffenbauer a, Volochayev R, Gardner P, Lee P, McLean J, Shenoi S, Rider L, Stevens A, Dey N. The Association Between Gingival Inflammation and Clinical Signs of Active Juvenile Dermatomyositis (JDM) [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/the-association-between-gingival-inflammation-and-clinical-signs-of-active-juvenile-dermatomyositis-jdm/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-association-between-gingival-inflammation-and-clinical-signs-of-active-juvenile-dermatomyositis-jdm/