Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: T cells are important among the several risk factors and immunological markers implicated in rheumatoid arthritis (RA). The goal of this study was to look for biological markers of cell exhaustion in CD4+ and CD8+ lymphocytes from RA patients in remission who were not receiving medication.
Methods: A cross-sectional, single-center study was carried out in a tertiary care center in Mexico City. We included 18-year-old patients who met the EULAR/ACR 2010 RA classification criteria. Patients were divided into three groups: G1) remission for 5 years without therapy with DMARDs and/or glucocorticoids; G2) remission on treatment, and G3) active patients. Pregnancy, active infection, cancer, and the presence of other autoimmune diseases (except Sjogren’s syndrome) were all exclusion criteria. Relevant clinical and serological parameters were recorded, and a univariate analysis was done with SPSS v29. Flow cytometry with Flow Jo v10 was used to analyze the expression of cell exhaustion markers (CTLA-4, LAG-3, PD-1, PD-L1, and Tim-3).
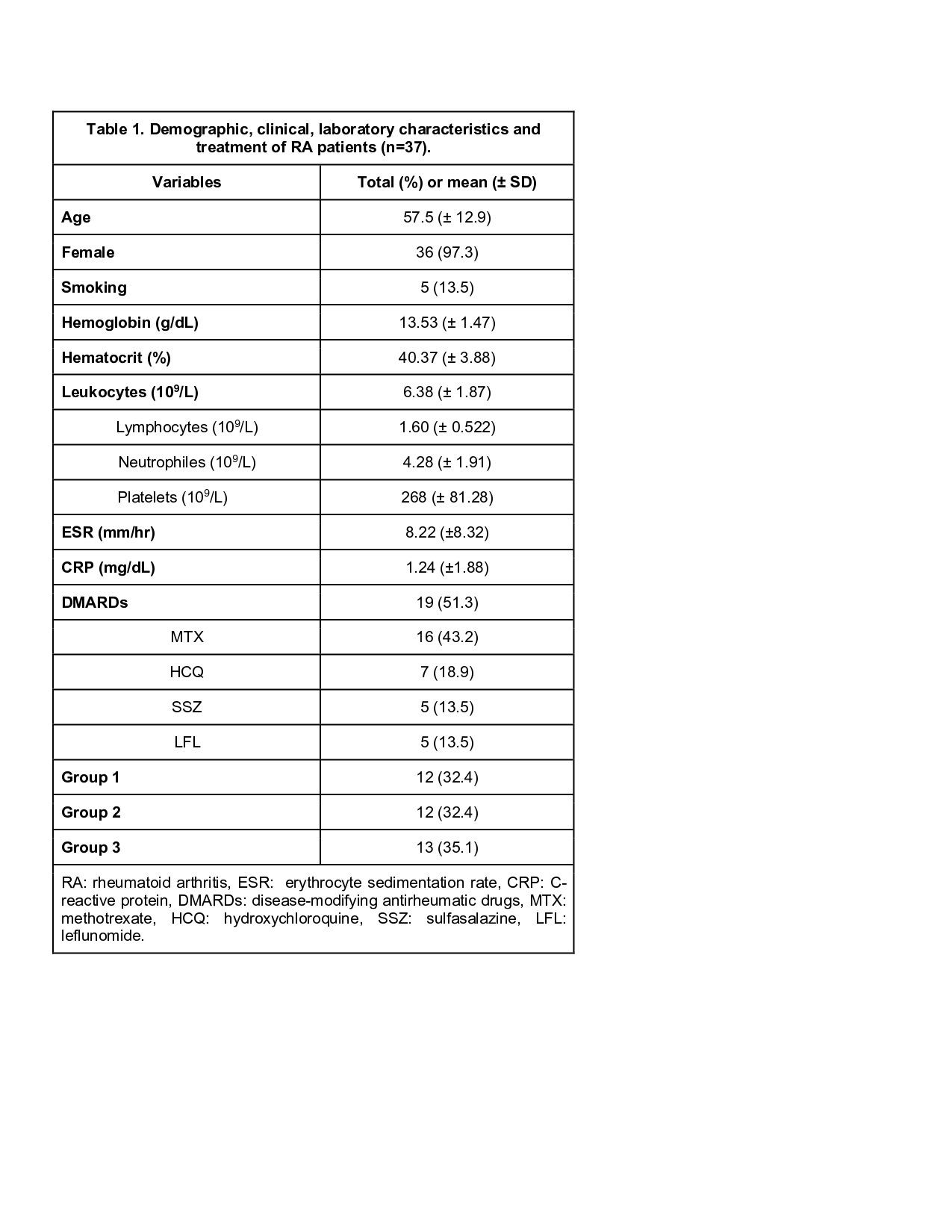
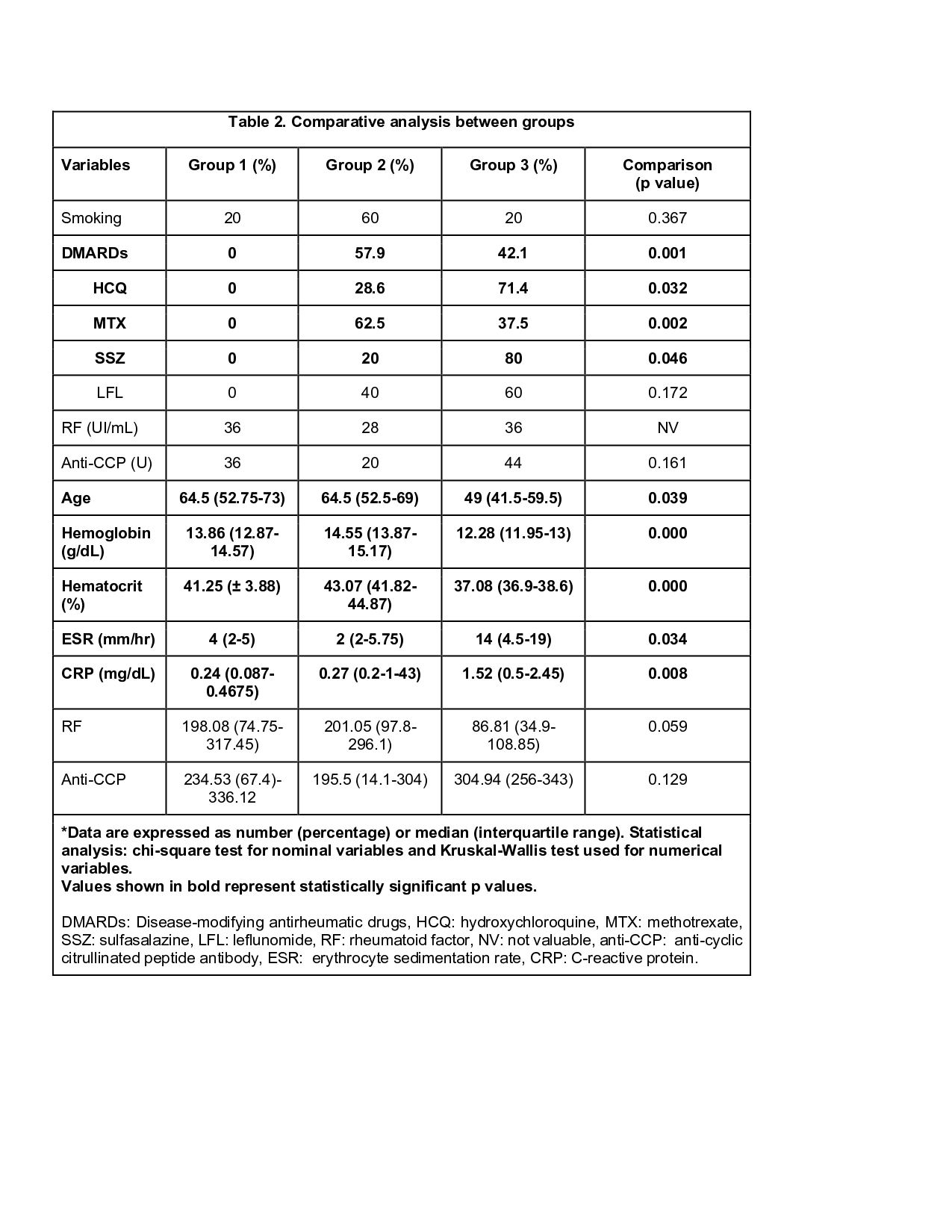
Results: We included 37 patients, 12 (32.4%) of whom were in remission without treatment (G1) and were paired with G2 (32.4%) and G3 (35.1%). The majority (97.3%) were female, the mean age was 57.5 (±12.9) years, and only 5 (13.5%) were smokers. Methotrexate (MTX) was used in 16, hydroxychloroquine (HCQ) in 7, sulfasalazine (SSZ) and leflunomide in 5 each. The mean ESR was 8.22 mm/hr (2-36), and the mean CRP was 1.24mg/dL (0.05-8.74), with no major differences detected between the three groups. When the use of DMARDs was analyzed by group, it was 0%, 57.9%, and 42.1% respectively (p< 0.001). HCQ use was higher in G3, with 0% vs 28.6% vs 71.4% (p=0.032), while SSZ and MTX were more frequent in G2-3, with 0% vs 20% vs 80% and 0% vs 62.5% vs 31.3%, respectively (p=0.046 and p=0.002). Other drugs showed no significant differences. Rheumatoid factor was positive in all patients, while anti-cyclic citrullinated peptide antibodies were positive in 90%, 71.4%, and 100%, respectively (p=0.161). (Table 1) When comparing numeric values between groups, G3 were younger patients and had higher values of ESR and PCR compared to other groups; with ages 64.5 (52.75-73) vs 64.5 (52.5-69) vs 49 (41.5-59.5) years (p=0.039), mean ESR of 4 (2-5) vs 2 (2-5.75) vs 14 (4.5-19) mm/hr (p=0.034), and mean CPR of 0.24 (0.0875-0.4675) vs 0.27 (0.2-1.43) vs 1.52 (0.5-2.455) mg/dL (p=0.008). Other variables were studied; however, no statistical significance was found. (Table 2)Cell exhaustion markers in CD4+ were higher in G2, except for PD-1, with LAG-3, PD-L1, ratio PD-1/PD-L1, and Tim-3 being significant (p=0.0052), whereas in CD8+, only the expression of PD-L1 was significantly different (p=0.0325) (Image 1). These findings suggest that G2 induces increased cell exhaustion, and treatment may be the primary determining factor. However, the limited sample size may have an impact on the findings.
Conclusion: To the best of our knowledge, this is the first study that assess multiple markers of cell exhaustion in RA patients, with expression perhaps related to remission and/or treatment. Further research with larger sample sizes is required to confirm our findings.
To cite this abstract in AMA style:
Jiménez-Soto R, llorente L, Lima G, Alanis Saenz L, Gomez Rodriguez A, Marin Lopez H, Cimé-Aké E, Jakez-Ocampo J. Senescence and Cell Exhaustion in CD4+ and CD8+ Lymphocytes in Rheumatoid Arthritis Patients in Remission Without Treatment [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/senescence-and-cell-exhaustion-in-cd4-and-cd8-lymphocytes-in-rheumatoid-arthritis-patients-in-remission-without-treatment/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/senescence-and-cell-exhaustion-in-cd4-and-cd8-lymphocytes-in-rheumatoid-arthritis-patients-in-remission-without-treatment/