Session Information
Date: Sunday, November 12, 2023
Title: (0380–0422) RA – Diagnosis, Manifestations, and Outcomes Poster I
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Chronic inflammation contributes to enhanced cardiovascular risk in rheumatoid arthritis (RA). Biologic disease modifying antirheumatic drugs (bDMARDs) control inflammation in many conventional synthetic DMARD non-responders and improve outcomes. We explored whether baseline bDMARD use may influence the impact of disease activity and systemic inflammation on long-term cardiovascular risk in RA.
Methods: We studied 4370 patients free of cardiovascular disease upon registration to An International Cardiovascular Consortium for people with RA (ATACC-RA) and followed prospectively. Outcomes included (a) major adverse cardiovascular events (MACE) defined as non-fatal myocardial infarction, non-fatal stroke, or cardiovascular death and (b) any ischemic cardiovascular events (CVE) comprising MACE, coronary revascularization, stable angina pectoris, transient ischemic attack and peripheral arterial disease with or without revascularization. Missing data were imputed using multiple imputation with 10 repetitions. Multivariable Cox models stratified by center evaluated the impact of disease activity (DAS28-CRP), inflammation (CRP), bDMARD use and their respective interactions on CVE risk after adjusting for age, gender, hypertension, diabetes, family history, smoking and total cholesterol to high-density lipoprotein ratio. Two corroborating sensitivity analyses were performed; the first included patients enrolled in the cohort on or after January 1, 2000, when bDMARD use became more prevalent. The second used inverse probability of treatment weights to balance differences in bDMARD treated and untreated patients.
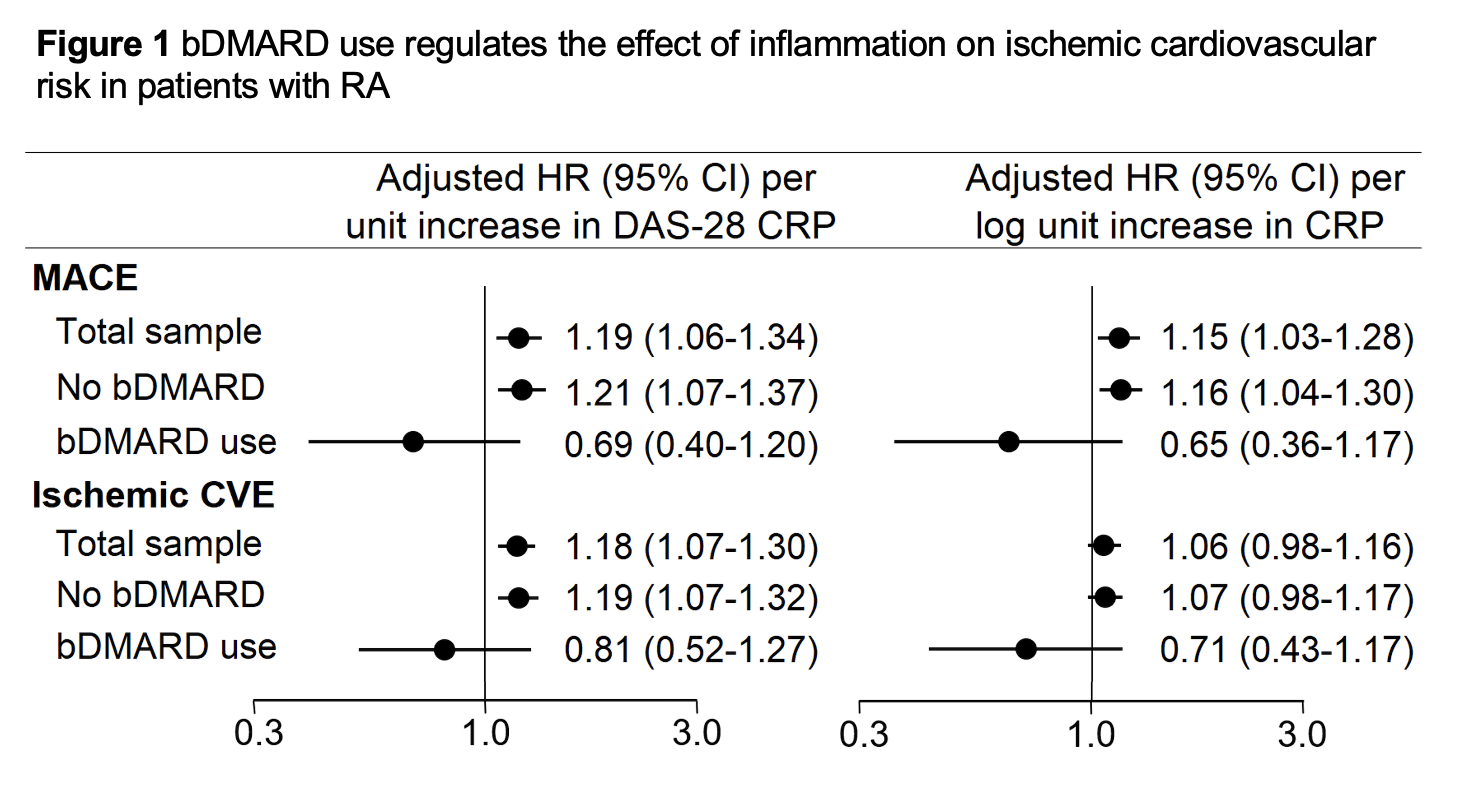
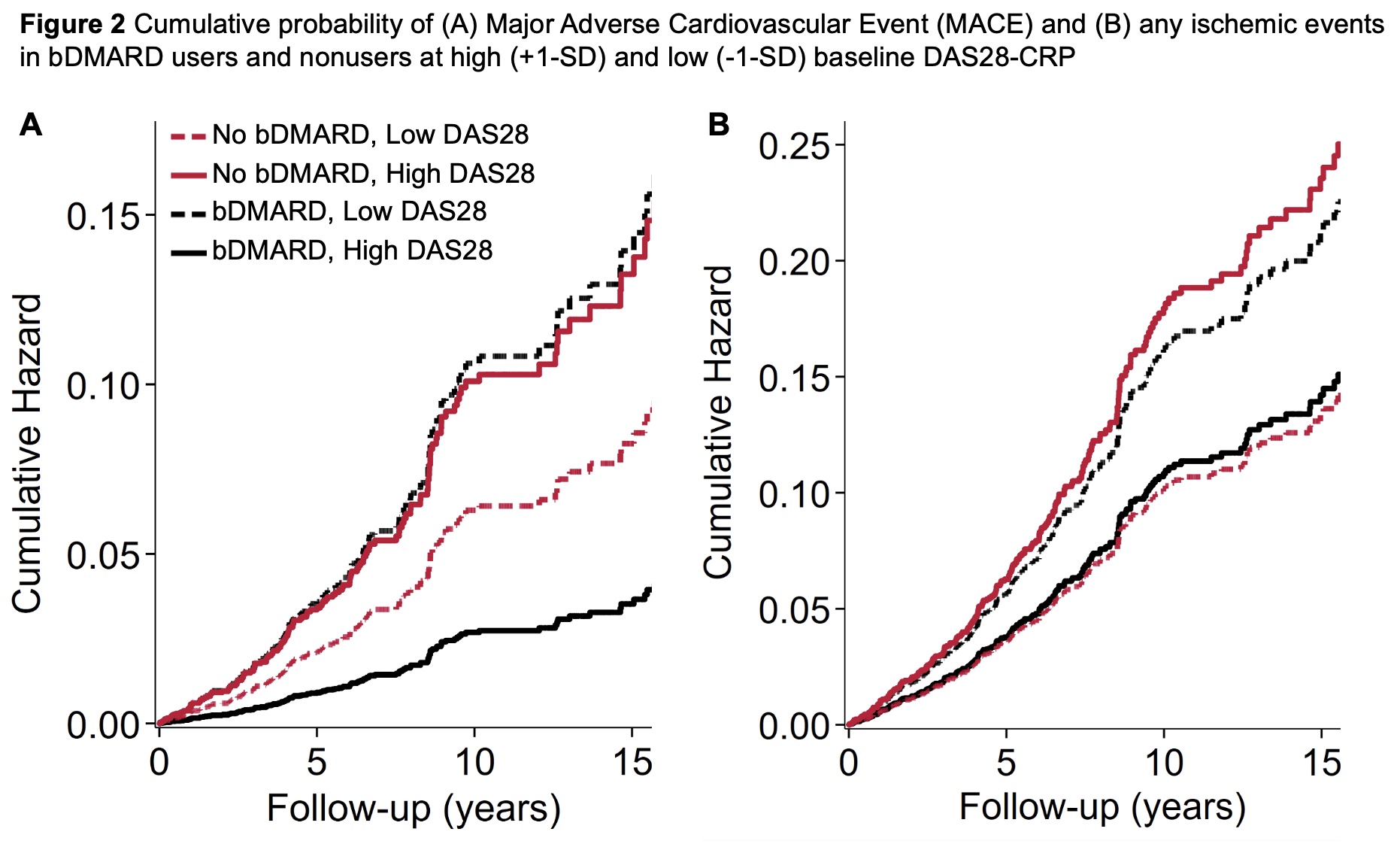
Results: Throughout 26,534 patient years, 239 first MACE and 362 total ischemic CVE were recorded. Among bDMARD nonusers, incidence of MACE and any ischemic CVE was 9.3 (95% CI 8.2-10.6) and 14.2 (12.8-15.8) events/1000PY. Rates for bDMARD users were [5.4 (95% CI 2.9-10.1) and 8.2 (5.0-13.6) events/1000PY. In the entire cohort, DAS-28 CRP and CRP(ln) associated with greater risk of MACE [(adjusted hazards ratio [aHR] 1.19 (95%CI 1.06-1.34), p=0.004 and HR 1.15 (1.02-1.28), p=0.017], while for all ischemic CVE the association was significant for DAS28-CRP [aHR 1.1 (95%CI 1.07-1.30)], but not CRP(ln) [aHR 1.06 (0.97-1.16)]. In bDMARD nonusers, higher DAS28-CRP and CRP(ln) associated with greater risk of MACE [aHR 1.21 (95%CI 1.07-1.37), p=0.002 and aHR 1.16 (1.04-1.30), p=0.009]. However, this was not the case in bDMARD users [p-for-interaction= 0.017 and 0.011 correspondingly, Figures 1 and 2]. In contrast, no significant interaction between DAS28-CRP or CRP and bDMARD use on any ischemic CVE risk was observed (p-for-interaction= 0.167 and 0.237 respectively). Both sensitivity analyses yielded similar results.
Conclusion:
Conclusion: Higher disease activity and systemic inflammation at baseline associated with greater risk of MACE in bDMARD nonusers but not in users. This may suggest the presence of additional bDMARD-specific benefits directly on atherosclerotic plaque —such as plaque stabilization— above and beyond effects on systemic inflammation.
To cite this abstract in AMA style:
Karpouzas G, Ormseth S, Van Riel P, Myasoedova E, Gonzalez-Gay M, Corrales A, Rantapää-Dahlqvist S, Sfikakis P, Dessein P, Tsang L, Hitchon C, El Gabalawi H, Pascual Ramos V, Contreras Yañez I, Colunga I, Galarza-Delgado D, Azpiri-López J, Rolefstad S, Semb A, Misra D, Hauge E, KITAS G. Biologic Use Regulates the Impact of Inflammation on Ischemic Cardiovascular Risk in Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/biologic-use-regulates-the-impact-of-inflammation-on-ischemic-cardiovascular-risk-in-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/biologic-use-regulates-the-impact-of-inflammation-on-ischemic-cardiovascular-risk-in-rheumatoid-arthritis/