Session Information
Date: Sunday, November 12, 2023
Title: (0229–0251) Metabolic & Crystal Arthropathies – Basic & Clinical Science Poster I
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Painful gout flares often lead to healthcare visits which, based on prior reports, results in the use of opioid therapy for flare management, despite opioids not being a preferred treatment. The use of opioids for flares raises concerns that uncontrolled gout may serve as a “gateway” to chronic opioid use. The objectives of this study were to: 1) compare the risk of initiating chronic opioid use in Veteran’s Health Administration (VHA) patients with and without gout, and 2) to examine determinants of initiating chronic opioid use in gout patients.
Methods: We performed a matched cohort study, identifying patients with gout using national VHA data from 1/1999-1/2015 based on ≥2 ICD-9 codes for gout (274.X). Gout cases were matched to patients without gout (up to 1:10) based on birth year, sex, and VA enrollment year, then followed from the index date (fulfillment of gout algorithm) until the earliest of incident chronic opioid use, death, or 5 years after the index date. Individuals with a fill of an opioid in the year prior to the index date were excluded. Chronic opioid use was defined as ³90 cumulative days’ supply with at least 2 dispenses occurring in a 6-month window with no gap >32 days. Associations of gout (vs. non-gout) with chronic opioid use were quantified using a cumulative hazard curve and multivariable Cox proportional hazards regression. Associations between patient characteristics and time-to-initiating chronic opioid use among patients with gout were examined in separate analyses. Covariates in both models included race, comorbidities, body mass index (BMI), and smoking status. In the gout-only model, additional covariates included age, sex, Rheumatic Disease Comorbidity Index (RDCI), time-varying serum urate (SU) control (average SU < 6 mg/dL in prior year) and urate-lowering treatment (ULT; ≥2 fills of ULT with ≥90 days covered by dispensing in prior year).
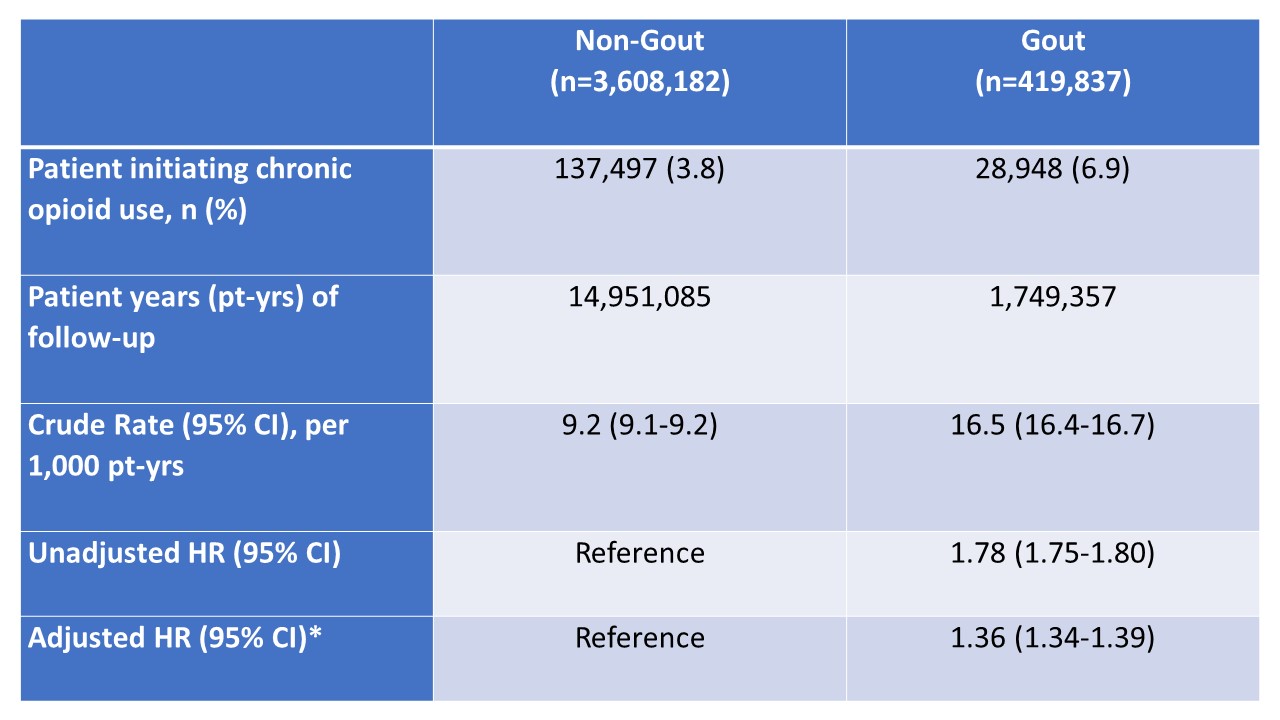
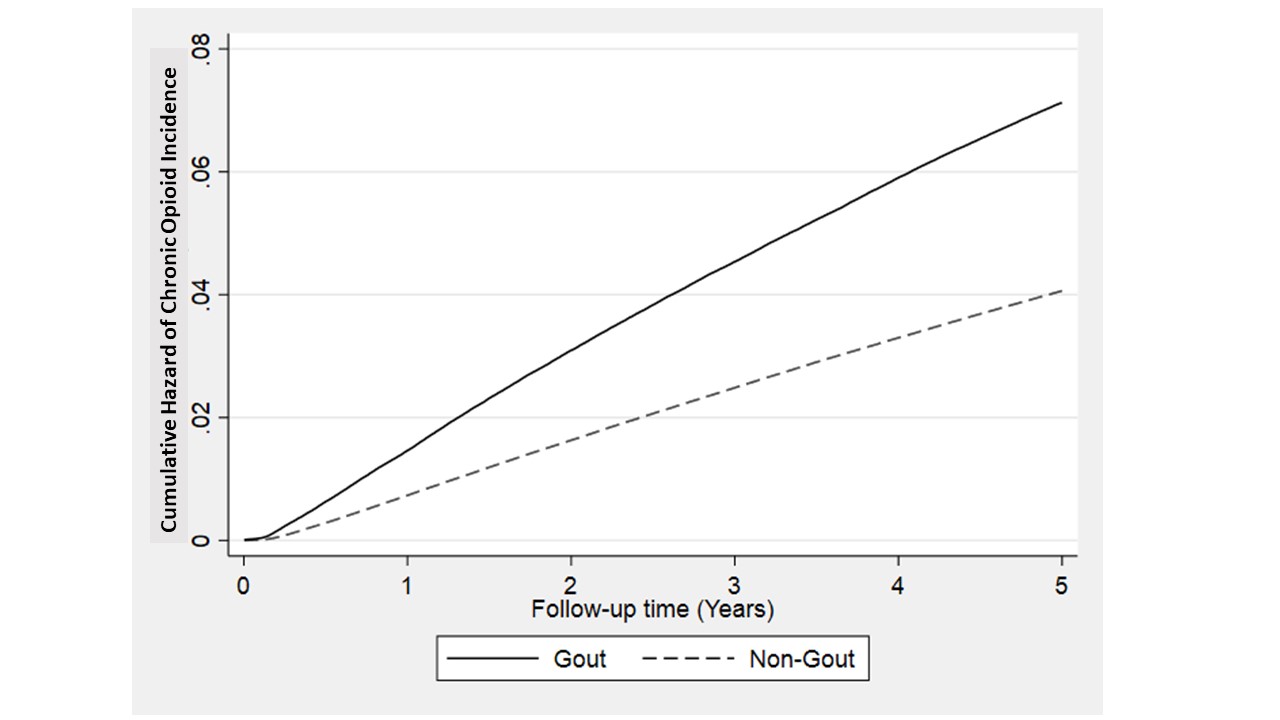
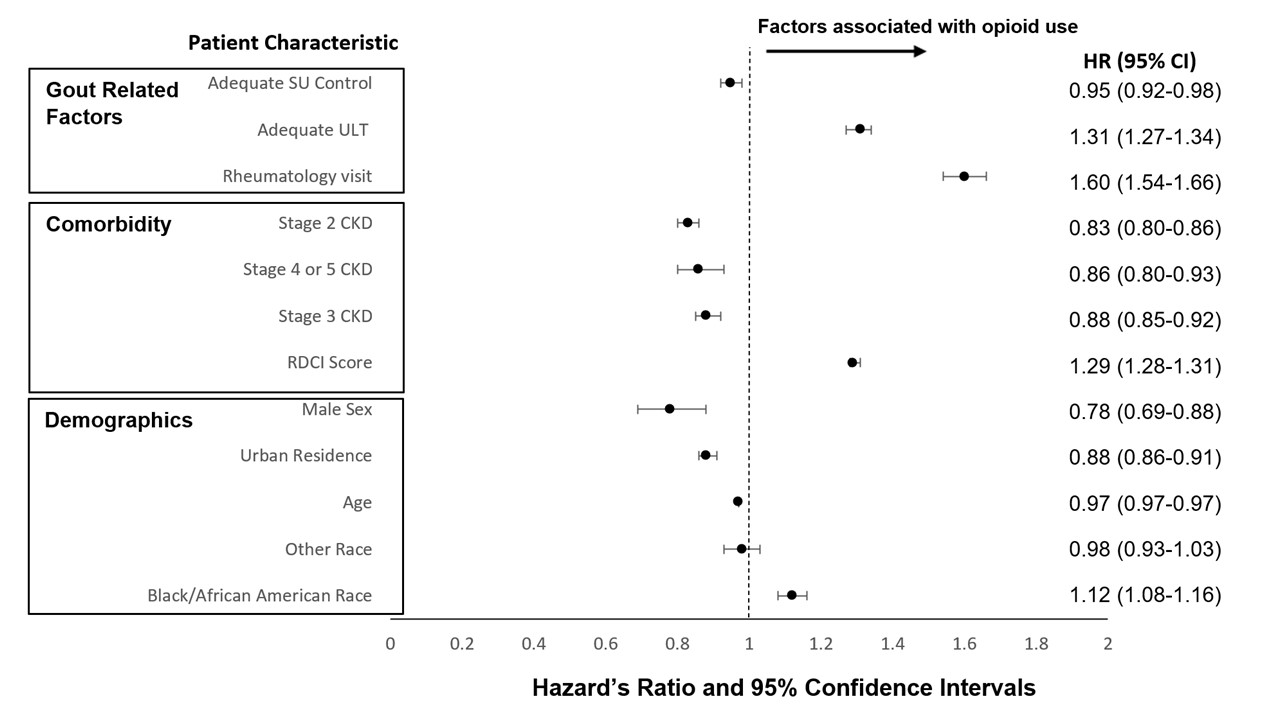
Results: Over 16.7 million patient-years of follow-up (median follow-up 5 years), 6.9% of gout patients initiated chronic opioids vs. 3.8% of non-gout patients (Fig. 1, Table 1). After adjusting for covariates, patients with gout were significantly more likely than non-gout patients to initiate chronic opioid use (aHR 1.36; 95% CI 1.34 to 1.39). Factors associated with gout-related chronic opioid exposure are summarized in Fig. 2.Among those with gout, factors positively associated with chronic opioid use included Black/African American race, comorbidities, ULT use, and rheumatology encounter. Factors negatively associated with chronic opioid use in those with gout included male sex, CKD, urban residence, SU control, age, and Asian, Native Hawaiian/Pacific Islander, and American Indian race.
Conclusion: In the VHA, we found that patients with gout were 36% more likely than those without gout to initiate chronic opioid use, after accounting for potential confounders, despite opioids not being recommended for management of gout flares. Associations between patient characteristics and time-to-initiating chronic opioid use highlight potential gaps in care, particularly among underserved Black/African American and rural populations as well as the potential for adequate urate control to reduce the risk of chronic opioid use in gout.
*Covariates include age, index year, race (Black/African American, Other, or Missing vs. White), BMI, smoking status (Former, Current, or Missing vs. Never), chronic lung disease, past myocardial infarction, cardiovascular disease, stroke, hypertension, diabetes, fracture, depression, stomach ulcer or cancer.
*All variables in multivariable model with p-value <0.05 are shown in the figure
White/Caucasian race was referent value; Other race includes composite of Asian, Native Hawaiian/Pacific Islander, and American Indian; Adequate ULT indicates ≥2 fills of ULT –AND- at least ≥90 days covered by dispensing; Adequate SU control indicates average SU <6 mg/dL; Age reported in years; Rheumatology visit reported as presence of any visit throughout follow up period; RDCI (rheumatic disease comorbidity index) including lung disease, myocardial infarction, other cardiovascular disease, stroke, hypertension, fracture, depression, diabetes mellitus, ulcer or stomach problem, and cancer
Abbreviations: urate lowering therapy (ULT), chronic kidney disease (CKD), serum urate (SU)
To cite this abstract in AMA style:
Helget L, England B, Roul P, Sayles H, Neogi T, O'Dell J, Mikuls T. Gout: A Gateway to Chronic Opioid Use? [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/gout-a-gateway-to-chronic-opioid-use/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/gout-a-gateway-to-chronic-opioid-use/