Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Herpes zoster (HZ) is a painful rash that is commonly known as shingles. People that had a primary infection caused by the varicella-zoster virus known as chicken pox can present herpes zoster at any age.1 The infection manifests as a vesicular rash with the characteristic of following a dermatomal pattern followed by postherpetic neuralgia. Herpes zoster is commonly observed in the elderly and immunocompromised populations such as patients with autoimmune diseases or malignancies. On average HZ incidence in a normal population is 1.2 to 4.9 cases per 1000 person per year; however, herpes incidence is multiplied in those with autoimmune diseases.2
Methods: We conducted a cross-sectional study that included consecutive patients with RD who were ≥ 18 years attending the rheumatology service in a northeast referral hospital in Mexico. We excluded patients who refused to participate. The following data was collected between December 2022 to May 2023: demographics, medical history, and RD diagnosis. We applied a paper-based questionnaire and reviewed medical records to identify HZ events in patients with RD, demographics, onset, recurrence, vaccination status, and hospital admissions related to HZ and HZ-related factors.
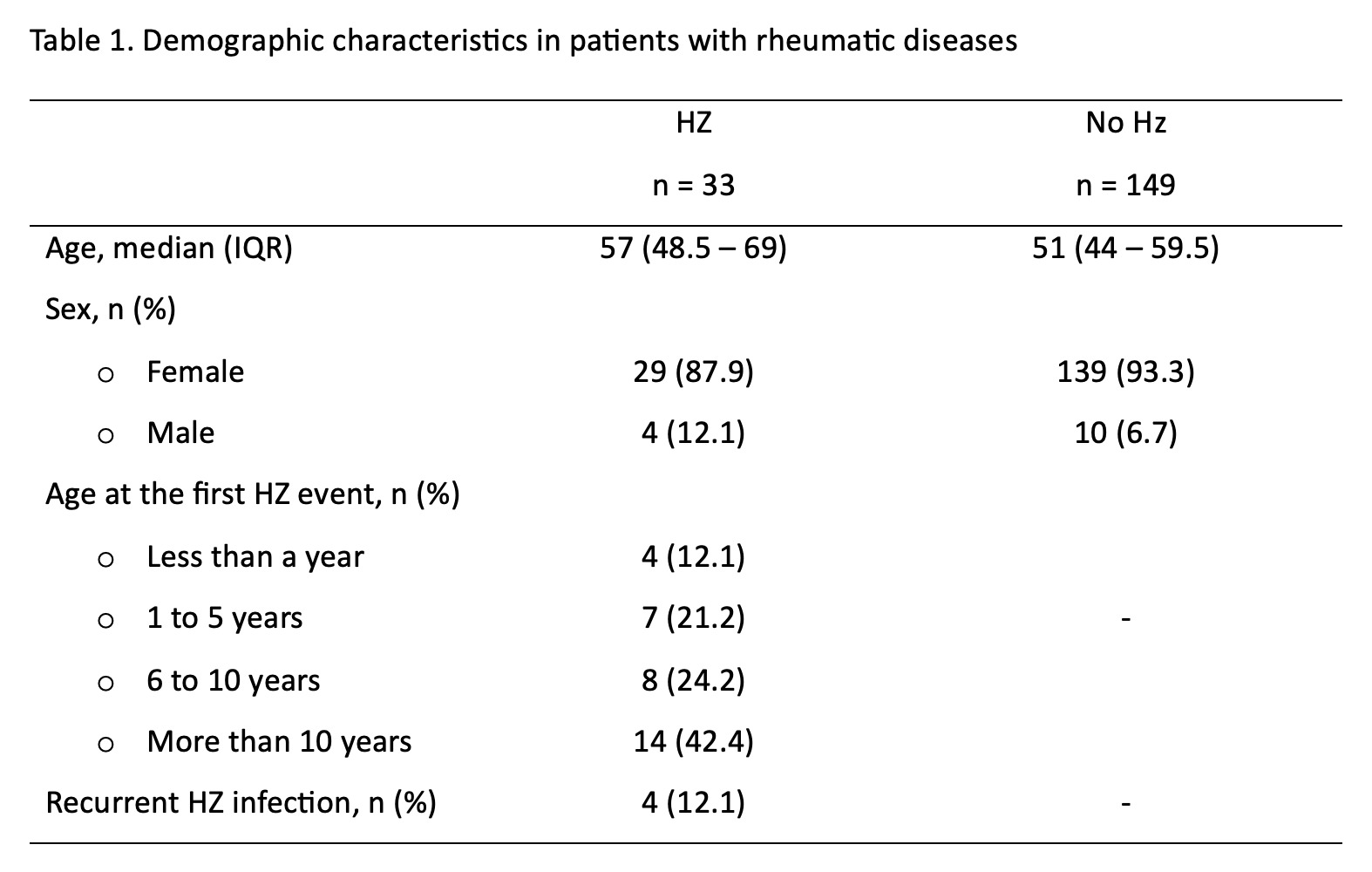
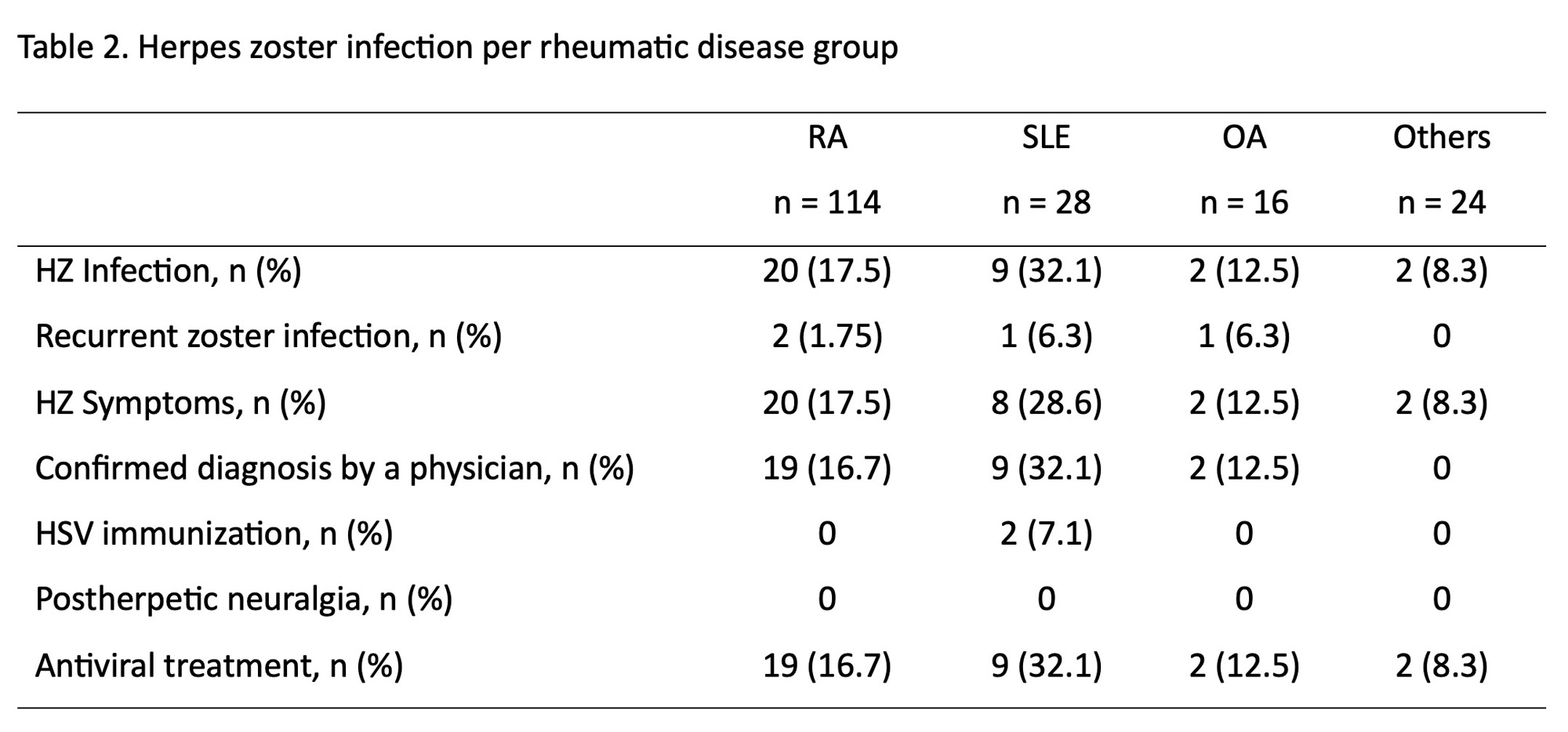
Results: A total of 182 patients with RD were screened for HZ. Patients with HZ had a median and IQR age of 57 (48.5 – 69). Thirty-three (18.13%) patients reported an HZ event; of which 14 (42.4) had their first HZ event over more than 10 years ago. Thirty-two (96.97%) were treated with antivirals, 3 (9.09%) were hospitalized due to severe disease, and 31 (93.94%) were not vaccinated against HZ. Regarding rheumatic diseases 9 (32.1) SLE patients, 20 (17.5) RA patients, and 2 (12.5%) OA patients had HZ. (See Tables 1 and 2).
Conclusion: Herpes zoster events are six folded in patients with rheumatic diseases. The prevalence of HZ-events is higher in patients with autoimmune diseases, specifically in those with SLE. The frequency of HZ events and severe disease can be prevented through vaccination; however, the vaccine may not be accessible to everyone.
1. Yun H, Yang S, Chen L, Xie F, Winthrop K, Baddley JW, et al. Risk of Herpes Zoster in Autoimmune and Inflammatory Diseases: Implications for Vaccination. Arthritis Rheumatol. 2016;68(9):2328-37.
2. Chen HH, Chen YM, Chen TJ, Lan JL, Lin CH, Chen DY. Risk of herpes zoster in patients with systemic lupus erythematosus: a three-year follow-up study using a nationwide population-based cohort. Clinics (Sao Paulo). 2011;66(7):1177-82.
To cite this abstract in AMA style:
Castillo-de la Garza R, Esquivel-Valerio J, Campos-Tinajero E, Carrazco Chapa A, García Arellano G, De Leon-Perez A, Gamez-Siller P, Galarza-Delgado D. Herpes Zoster Prevalence in Patients with Rheumatic Diseases [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/herpes-zoster-prevalence-in-patients-with-rheumatic-diseases/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/herpes-zoster-prevalence-in-patients-with-rheumatic-diseases/