Session Information
Session Type: Poster Session A
Session Time: 6:00PM-7:00PM
Background/Purpose: Juvenile systemic sclerosis (jSSc) is a rare autoimmune, chronic, multisystem, connective tissue disease characterized by progressive tissue fibrosis of the skin and internal organs. To date, there have been few published studies on the clinical features of jSSc in East Asian population. The aim of this study was to describe clinical and laboratory characteristics at diagnosis, therapeutic drugs, and prognosis of jSSc at a single, tertiary-care hospital in South Korea.
Methods: The study was a retrospective analysis of jSSc patients having age of onset less than 16 years and underwent evaluations at Seoul national university hospital, between January 1992 and July 2022. All patients met the PReS/ACR/EULAR provisional classification criteria for jSSc, and patients with localized scleroderma (morphea) was excluded.
Results: Among the 13 jSSc patients, 8 patients (62%) were female, and the mean age of symptom onset was 10 years (range 2–13 years). The median time from onset of symptoms to diagnosis was 2 years (range 0.4–5 years). Proximal skin sclerosis (13 patients, 100%), Raynaud’s phenomenon (RP) (11, 85%), and sclerodactyly (9, 69%) were presented at the time of diagnosis. However, the first symptom patients reported the most was RP which was present in 10 patients (77%). In comparison, proximal skin sclerosis was present only in 5 (38%).
A total of 13 patients (100%) had positive result of ANA test. Anti Scl-70 antibody (ab) was positive in 7 (54%) out of 13 patients tested, and anti RNP ab was positive in 2 out of 11 patients tested. Autoantibody tests including, RF, anti CCP ab, anti-dsDNA ab, anti-Smith ab, ACA, ANCA, and ASCA were performed, but all were negative.
At the time of diagnosis, 5 patients showed mild restrictive pattern on pulmonary function tests (PFT) or chest CT findings of interstitial lung disease, of which 3 felt dyspnea on exertion, and 1 out of 3 complained chronic cough. In the other 2, there was no subjective dyspnea despite abnormal findings.
Glucocorticoids were the most prescribed drug as an initial therapy, which was used in 8 patients, followed by Methotrexate in 6 patients. As a second-line therapy, 5 patients used MMF and 2 patients used CPM to control severe symptoms. For severe RP, 12 patients took calcium channel blockers.
During follow-up, 3 patients developed lung disease, 1 patient had impaired renal function, and 1 patient developed heart disease.
Conclusion: In the early phase of jSSc, the diagnosis is very difficult due to insidious and subtle onset of skin changes. In our population, proximal skin sclerosis, which is crucial in diagnosis of jSSc, was not present in the early phase of disease. Considering the importance of timely diagnosis and treatment in the early phase of disease, clinical suspicion is essential for diagnosis of jSSc with RP especially when ANA is positive. Since all autoantibodies other than ANA were negative in 38% of patients, jSSc cannot be excluded even if all autoantibodies other than ANA are normal in children with RP, and close physical examination is required. PFT and chest CT should be performed at diagnosis as 38% of patients showed lung involvement at the initial evaluation with or without respiratory symptoms.
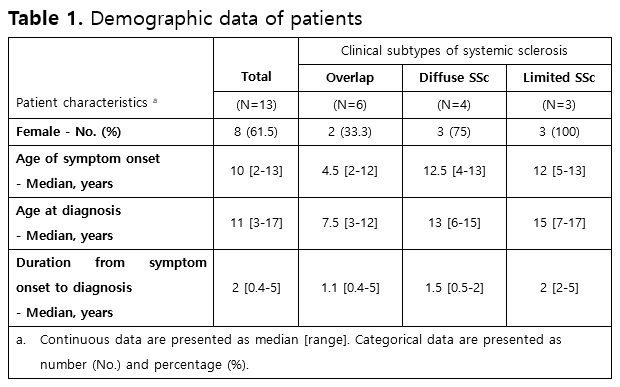 Table 1. Demographic data of patients
Table 1. Demographic data of patients
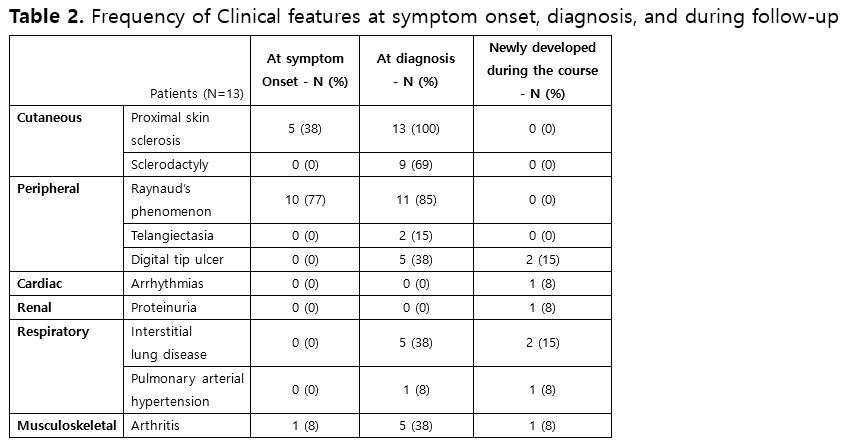 Table 2. Frequency of clinical features at symptom onset, diagnosis, and during follow-up
Table 2. Frequency of clinical features at symptom onset, diagnosis, and during follow-up
To cite this abstract in AMA style:
Jeong J, Kim M, Jung J, Lim S, Kim S. Clinical Characteristics of Juvenile Systemic Sclerosis in Korea: A 30-year Single Center Study [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 4). https://acrabstracts.org/abstract/clinical-characteristics-of-juvenile-systemic-sclerosis-in-korea-a-30-year-single-center-study/. Accessed .« Back to 2023 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-characteristics-of-juvenile-systemic-sclerosis-in-korea-a-30-year-single-center-study/
