Session Information
Date: Friday, March 31, 2023
Title: Poster Breakout 4 - JDM & Scleroderma: Clinical & Therapeutic Aspects
Session Type: Breakout Session
Session Time: 4:30PM-5:00PM
Background/Purpose: Cardiac disease is a major cause of morbidity and mortality in children with SLE and SSc. Various studies have demonstrated an association between duration of disease and abnormalities on cardiac magnetic resonance imaging (CMR) in pediatric rheumatic conditions. CMR may be complementary to echocardiogram as it assesses edema and fibrosis, as well as right ventricular ejection fraction (RV EF). We assessed additional cardiac inflammation/damage data gleaned from children with SLE and SSc during times of cardiac symptomatology.
Methods: We performed an IRB-approved query of our CMR database (patients 2014-2022) and abstracted data on 11 children (16 CMRs) with SLE-spectrum or SSc. We recorded echocardiographic findings from the most recent echo prior to CMRs. Echo parameters included tricuspid regurgitation (TR; jet >2.5 m/sec), ventricular dysfunction (LV and RV), and pericardial effusion (PCE). CMR evaluated LV and RV function, myocardial fibrosis, myo/pericarditis, and PCE. We used STIR and T2 map sequences to determine edema indicative of myo/pericarditis and delayed enhancement sequence for fibrosis assessment. SLEDAI score was used to assess patient disease activity at the time of CMR.
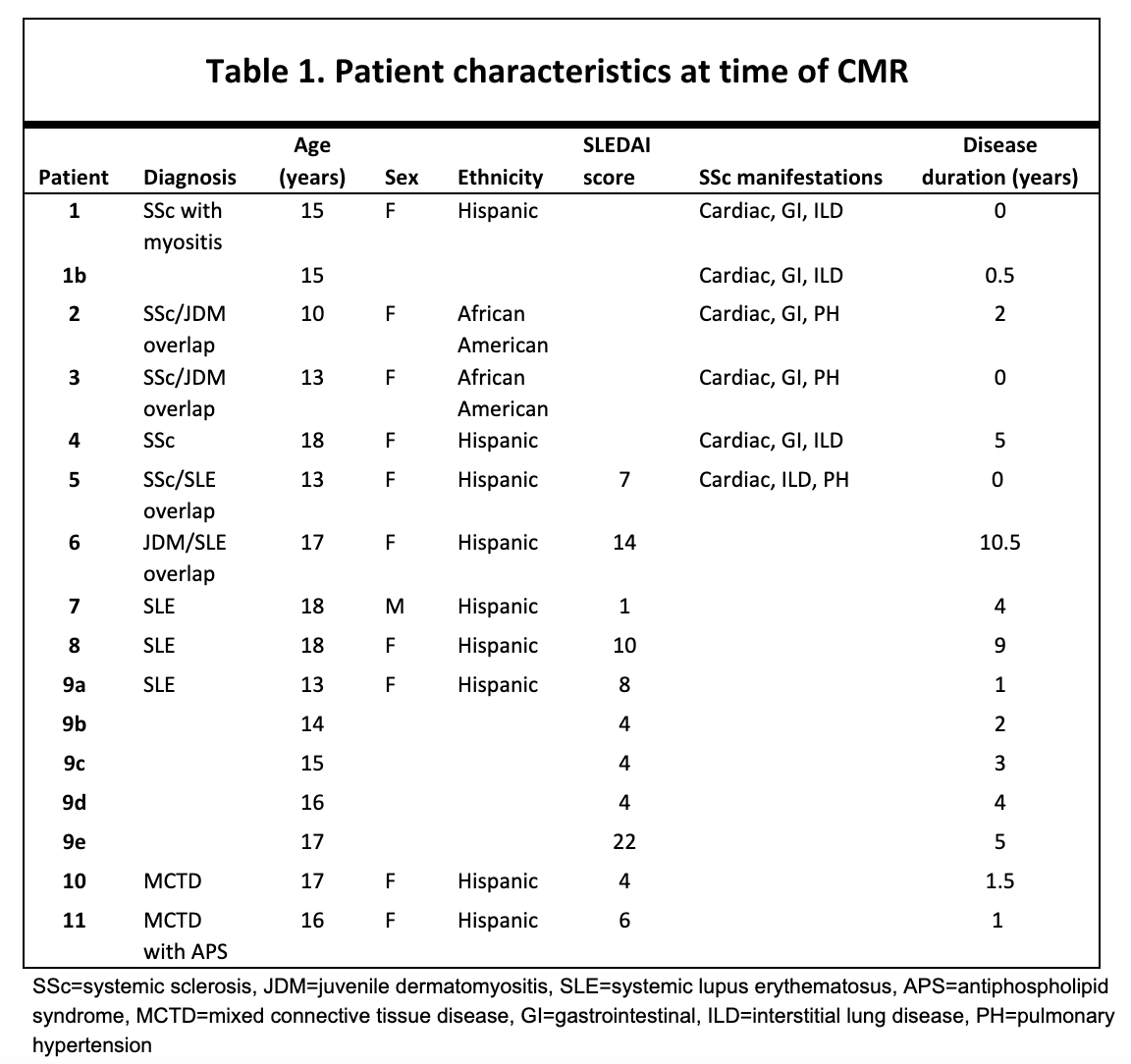
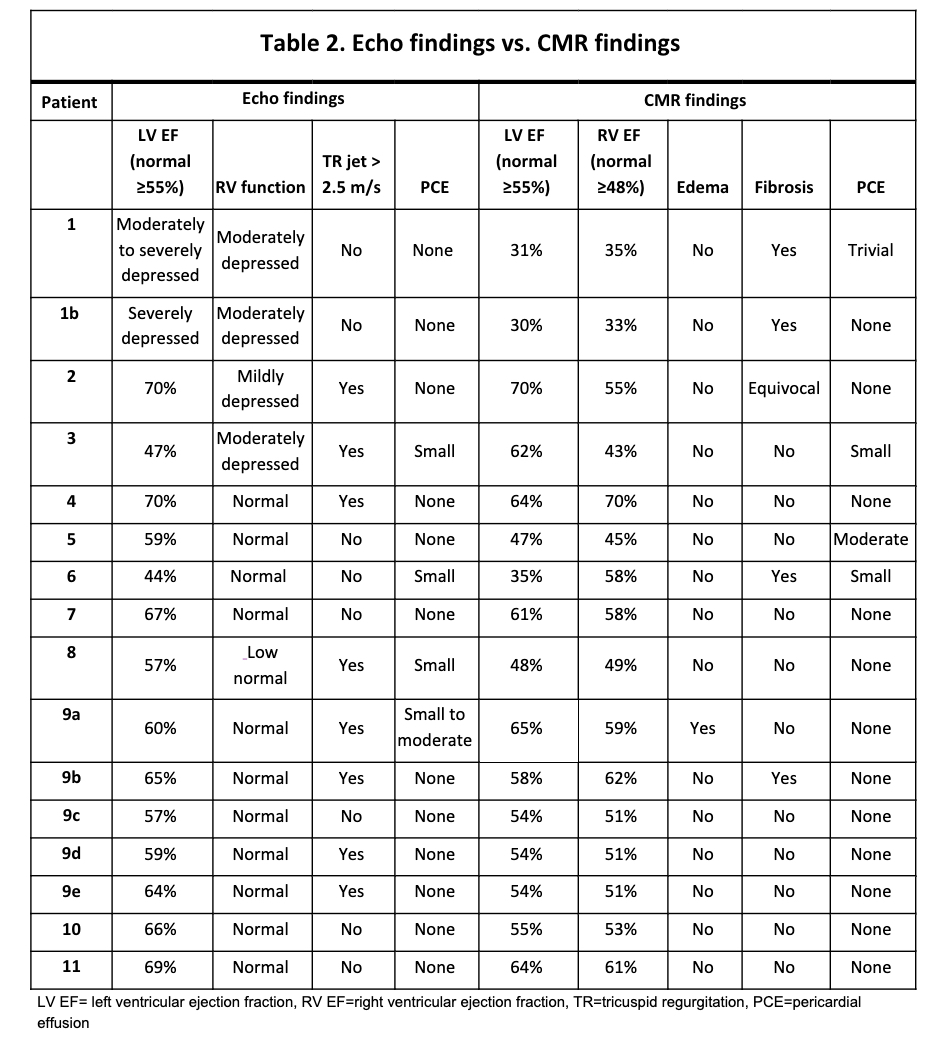
Results: Patients median age at time of CMR (n=16 scans) was 16 years (range=10-18), and median disease duration was 1.5 years (range=0-10). 82% were female, 82% were Hispanic/Latino, and 18% were Black/African American. Median SLEDAI score of patients with SLE-spectrum disease at time of CMR was 7 (range=1-14). Two of the seven patients with SLE-spectrum disease (28.5%) had renal manifestations at time of CMR, and none had CNS disease. Among the five patients with SSc, three (60%) had interstitial lung disease (ILD), three (60%) had pulmonary hypertension (PH), and four (80%) had GI involvement (Table 1). Thirteen (81%) of the 16 echocardiograms done prior to CMR demonstrated significant abnormality (Table 2). CMRs were performed in three other patients with normal echos, one of whom who was receiving PH therapy, one with cardiac symptoms and elevated cardiac enzyme, and one with abnormal T waves concerning for myocarditis. Additional cardiac abnormalities were identified on CMR in seven (44%) of the scans: one (6%) with edema, four (25%) with fibrosis, one (6%) with LV/RV dysfunction not seen on echo, and one (6%) with RV dysfunction not seen on echo. LV function was worse on CMR as compared to echo in 11 (79%) of the cases (Table 2). CMRs led to escalation in immunomodulatory therapy in all three patients with edema or fibrosis on CMR. Of the patients with abnormalities on CMR, one showed resolution of fibrosis on subsequent imaging, and the others had stable depressed function on repeat echo or CMR.
Conclusion: CMR performed in children with SLE and SSc revealed cardiac edema and fibrosis as well as lower LV/RV function than detected on echocardiography. Findings of cardiac fibrosis and/or edema led to a change in care in a third of patients. Future directions may include assessing CMR as an early screening tool, especially in patients with SSc who may have rapidly progressive and at times fatal cardiac manifestations.
To cite this abstract in AMA style:
Rae M, Doan T, Muscal E. Cardiac Magnetic Resonance Imaging in Children with Systemic Lupus Erythematosus and Scleroderma Spectrum Disorders: A Single Center Experience [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 4). https://acrabstracts.org/abstract/cardiac-magnetic-resonance-imaging-in-children-with-systemic-lupus-erythematosus-and-scleroderma-spectrum-disorders-a-single-center-experience/. Accessed .« Back to 2023 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/cardiac-magnetic-resonance-imaging-in-children-with-systemic-lupus-erythematosus-and-scleroderma-spectrum-disorders-a-single-center-experience/