Session Information
Session Type: Poster Session C
Session Time: 1:00PM-3:00PM
Background/Purpose: Early detection and assessment of Knee Osteoarthritis (KOA) prognostic factors are crucial for developing management and treatments that aim at prevention of irreversible damage to the knee joint leading to arthroplasty. It has recently been shown that trabecular bone texture (TBT) analysis of conventional X-Rays is an efficient imaging biomarker capable of identifying patients at high risk of developing KOA progression, permitting better approaches for clinical management [1–3].
The purpose of this study was to investigate whether short term variations in tibial subchondral TBT analysis could help predict KOA progression.
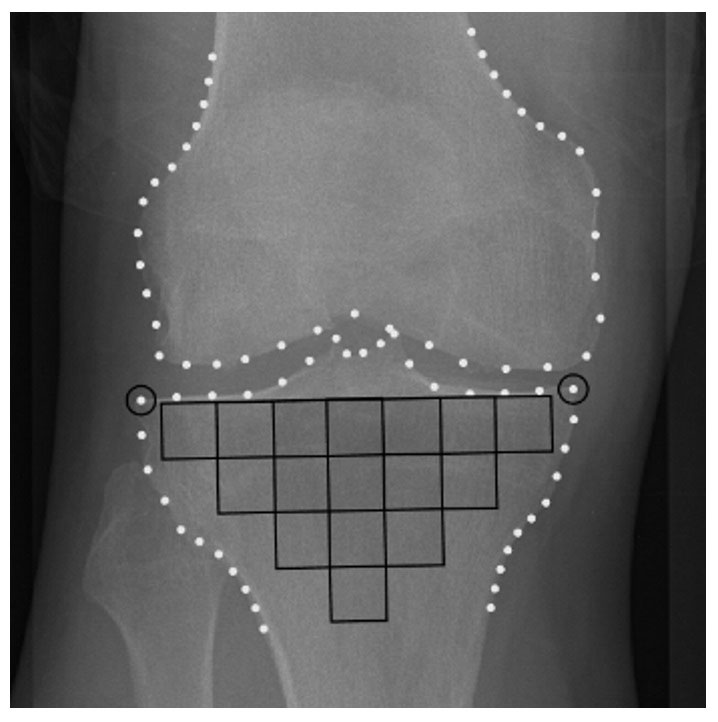
Methods: This study included 1719 patients from the Osteoarthritis Initiative cohort. Cases were defined as patients with an increased medial joint space narrowing (JSNM) score from baseline to 48-month follow-up. The baseline to 24-month variations (∆) in the TBT parameters of the subchondral zone of the tibia (Figure 1) were computed using the quadratic variations estimator [1].
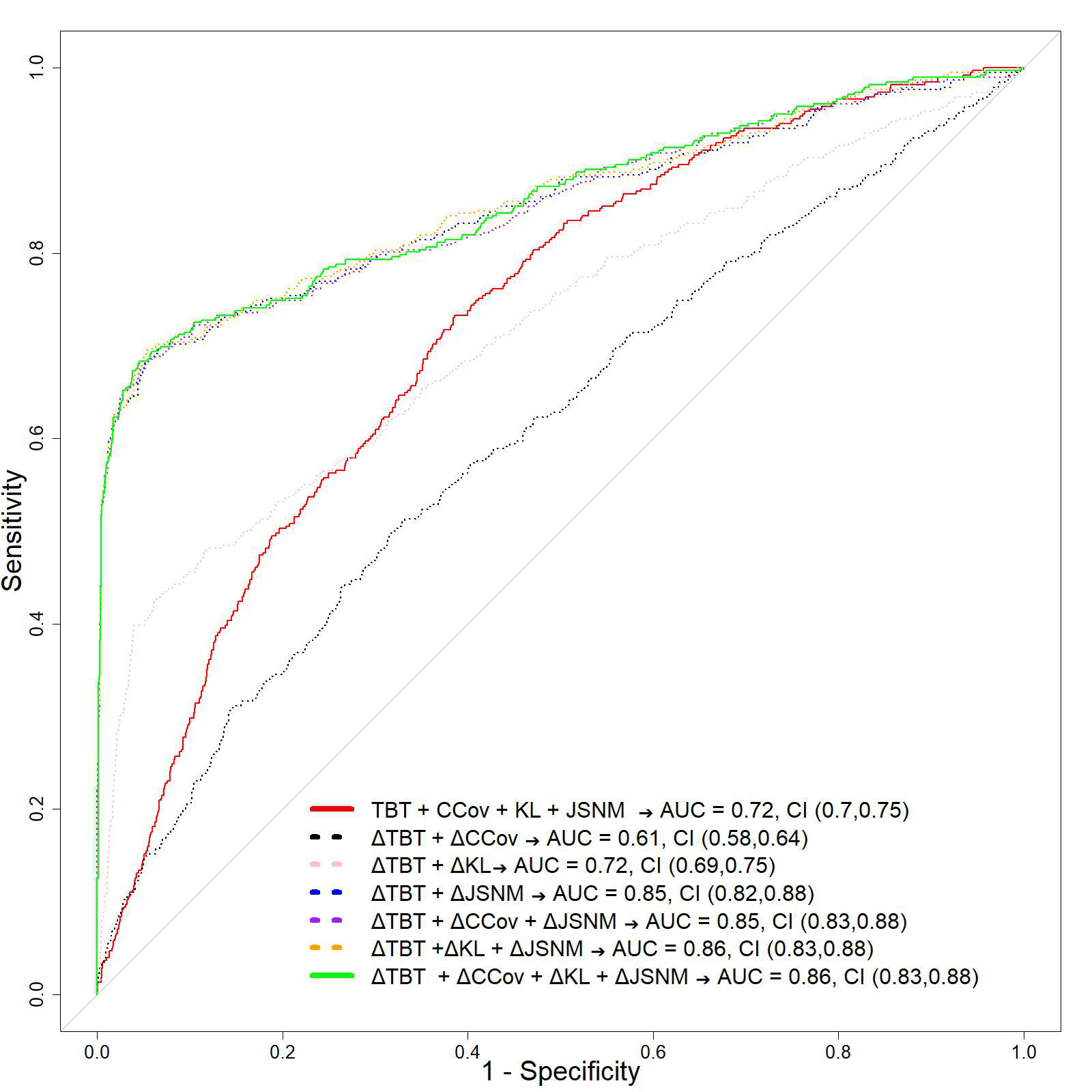
Several logistic regression models were developed to evaluate the performance of predicting KOA progression in 48 months when associating the TBT variations with a set of clinical and radiographic parameters, namely CCov (sex, age, BMI and WOMAC pain), KL and JSNM scores.
Model 1: TBT+CCov+KL+JSNM (Reference model [3])
Model 2: ∆TBT+∆CCov
Model 3: ∆TBT+∆KL
Model 4: ∆TBT+∆JSNM
Model 5: ∆TBT+∆CCov+∆JSNM
Model 6: ∆TBT+∆KL+∆JSNM
Model 7: ∆TBT+∆CCov+∆KL+∆JSNM
The area under the receiver operating characteristic curve (AUC) was used to determine the most predictive model.
Results: The proposed prediction models, based on ∆TBT, ∆CCov, ∆KL and ∆JSNM, achieved an AUC of 0.86, and outperformed a reference model, based exclusively on baseline readings which achieved an AUC of 0.72 (Figure 2). This improvement was mainly related to the variations of both TBT descriptors and JSNM scores. Including WOMAC pain scores did not show any improvement on the retained model.
Conclusion: The proposed model, involving radiographic TBT variations within 24 months, improved the capacity of predicting KOA progression over 48 months.
References
1. Janvier T, Jennane R, Valery A, Harrar K, Delplanque M, Lelong C, et al. Subchondral tibial bone texture analysis predicts knee osteoarthritis progression: data from the Osteoarthritis Initiative. Osteoarthritis and Cartilage. 2017;25:259–66.
2. Kraus VB, Collins JE, Charles HC, Pieper CF, Whitley L, Losina E, et al. Predictive Validity of Radiographic Trabecular Bone Texture in Knee Osteoarthritis: The Osteoarthritis Research Society International/Foundation for the National Institutes of Health Osteoarthritis Biomarkers Consortium. Arthritis & Rheumatology (Hoboken, NJ). 2018;70:80–7.
3. Almhdie-Imjabbar A, Nguyen K-L, Toumi H, Jennane R, Lespessailles E. Prediction of knee osteoarthritis progression using radiological descriptors obtained from bone texture analysis and Siamese neural networks: data from OAI and MOST cohorts. Arthritis Research & Therapy. 2022;24:66.
To cite this abstract in AMA style:
Almhdie-Imjabbar A, TOUMI H, ZERZOUF Z, LESPESSAILLES E. Short-term Variations in Subchondral Tibial Bone Texture of Conventional X-Rays Predicts Knee Osteoarthritis Progression [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/short-term-variations-in-subchondral-tibial-bone-texture-of-conventional-x-rays-predicts-knee-osteoarthritis-progression/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/short-term-variations-in-subchondral-tibial-bone-texture-of-conventional-x-rays-predicts-knee-osteoarthritis-progression/