Session Information
Session Type: Poster Session C
Session Time: 1:00PM-3:00PM
Background/Purpose: Idiopathic inflammatory myopathies (IIM) are a group of autoimmune diseases characterized by autoantibodies plus infiltration of leukocytes into muscles and/or the skin, leading to destruction of blood vessels and muscle fibers, chronic muscle weakness and fatigue. While complement-mediated destruction of capillary endothelium in muscle and skin are implicated in juvenile and adult-onset dermatomyositis, the genetic contribution of complement C4 in IIM pathology remains unknown.
Methods: We elucidated the gene copy number (GCN) variations of total C4 (C4T), C4A and C4B, long and short genes in 1,644 Caucasian IIM patients, plus 3,526 matched healthy controls from the US and Europe using TaqMan-based realtime PCR or Southern blot analyses. Plasma complement protein levels were measured by single radial immunodiffusion.
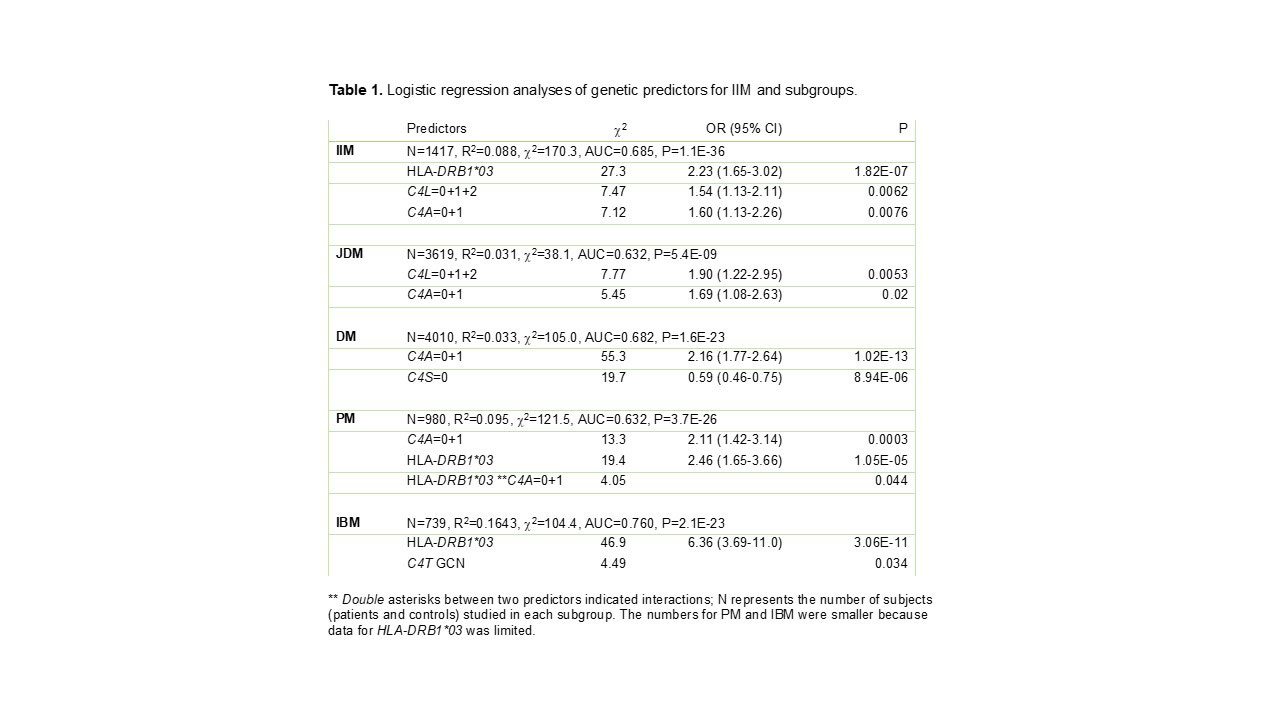
Results: Low GCN of C4T (C4T=2+3) and C4A deficiency (C4A=0+1) were strong risk factors for IIM with odds ratios and 95% confidence intervals of 2.58 (2.28-2.91), p=5.0×10-53 for C4T; and 2.82 (2.48-3.21), p=7.0×10-57 for C4A deficiency. Contingency analyses showed that among patients with C4A deficiency, HLA-DRB1*03 became insignificant as a risk factor in IIM except for inclusion body myositis, in which 98.2% had HLA-DRB1*03 with an OR of 11.02 (1.44-84.4), p=0.0012. Multivariate logistic regression analyses were also performed for genetic risk factors of IIM and subgroups with healthy controls (Table 1). Predictors were chosen from results of individual analyses and added to logistic regression models. Those with p-values >0.05 were removed stepwise and those with p-value < 0.05 retained. In JDM and DM, C4A deficiency and C4 gene size were independent and significant risk factors. In PM and IBM, both HLA–DRB1*03 and C4 gene copy numbers were significant risk factors. In PM, HLA–DRB1*03 and C4A deficiency interacted to confer risk. In IBM, HLA–DRB1*03 was a very strong risk factor with contributions by continuous GCN variation of C4T. Intra-group analyses of IIM patients for C4 protein levels and IIM-related autoantibodies revealed that those with anti-Jo-1 or with anti-PM/Scl autoantibodies had significantly lower C4 concentrations than those without these autoantibodies.
Conclusion: In terms of genetic risk factors complement C4A deficiency was relevant for JDM and DM, while HLA-DR3 was important for IBM, and both C4A deficiency and HLA-DR3 contributed to PM.
To cite this abstract in AMA style:
Zhou D, King E, Rothwell S, Kryštůfková O, Notarnicola A, Coss S, Aziz R, Miller K, Dang A, Yu G, Drew J, Lundstrom E, Pachman L, Mamyrova G, Curiel R, Paepe B, Bleecker J, Payton A, Ollier W, O'Hanlon T, Targoff I, Flegel W, Sivaraman V, Oberle E, Akoghlanian S, Driest K, Spencer C, Wu Y, Nagaraja H, Ardoin S, Chinoy H, Rider L, Miller F, Lundberg I, Padyukov L, Vencovský J, Lamb J, Yu C. Intricate Roles of Low Gene Copy Numbers for Complement C4, C4A Deficiency and HLA-DRB1*03 as Genetic Risk Factors for Myositis, Its Subgroups and Autoantibodies [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/intricate-roles-of-low-gene-copy-numbers-for-complement-c4-c4a-deficiency-and-hla-drb103-as-genetic-risk-factors-for-myositis-its-subgroups-and-autoantibodies/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/intricate-roles-of-low-gene-copy-numbers-for-complement-c4-c4a-deficiency-and-hla-drb103-as-genetic-risk-factors-for-myositis-its-subgroups-and-autoantibodies/