Session Information
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: Autoimmune conditions appear to cluster in families, as may be expected by shared genetic risk factors in conditions such as rheumatoid arthritis (RA), autoimmune thyroiditis (AITD), celiac disease, and systemic lupus erythematosus (SLE). However, these conditions are polygenic, individual risk alleles have small effect sizes, and only a handful of alleles are shared across diseases. There are limited data on how to consider risk for autoimmune diseases among family members with RA. The objective of this study was to determine the risk of developing AITD, celiac, and SLE among first-, second-, and third- degree relatives (FDR, SDR, TDR) of RA patients.
Methods: This study was performed in the Utah Population Database (UPDB) containing genealogical data from the 1850s to modern day descendants. We analyzed UPDB genealogy data linked to in- and outpatient diagnosis code data from the University of Utah Health Sciences Center (UUHSC) electronic health record data from 1994-2020. International classification of diseases (ICD) 9th and 10th revision data were extracted on RA, AITD, celiac, inflammatory bowel disease (IBD), and SLE for RA patients and FDR, SDR and TDRs. Cases were defined using ≥1 diagnosis code. Odds ratios (OR) were estimated by comparing the number of autoimmune cases among relatives of RA patients to the expected cohort-matched population rates estimated using linked UUHSC EHR data. We calculated OR for RA among relatives of RA patients as a positive control; IBD served as a negative control.
Results: We studied 5,603 subjects with RA and 18,844 first-, 37,413 second-, and 78,169 third-degree relatives with linked UUHSC data. Among FDRs of RA subjects, we observed a significantly higher risk of AITD (OR 1.28, 95% CI 1.08. 1.50), celiac (OR 1.51, 95% CI 1.18, 1.92) and SLE (OR 1.34, 95% CI 1.11, 1.59) compared to population rates (Figure). Among the autoimmune conditions, only SLE had an increased risk among SDRs of RA patients. No significant increased risk for AITD, celiac or SLE was observed among TDRs compared to the overall population. The OR for FDRs of RA patients was 2.23 (95% CI 2.1-2.4), OR 1.37 (95% CI 1.3, 1.5) for SDRs, in line with prior studies. Rates of IBD among relatives of RA patients were similar to population rates.
Conclusion: Results from this unique dataset linking genealogy with phenotypic data in a large population suggest that a lower threshold for screening FDRs, i.e. the siblings, offspring, and parents of RA subjects, is warranted among relatives who exhibit signs or symptoms for AITD, celiac or SLE. Our data do not support a higher need to screen for these autoimmune conditions among TDRs, e.g. first cousins, of RA patients.
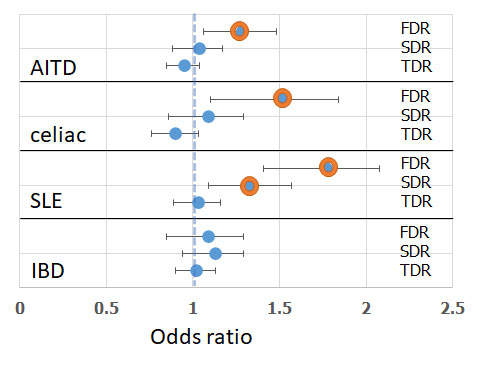 Figure. Risk of autoimmune thyroiditis (AITD), celiac, systemic lupus erythematosus (SLE), and inflammatory bowel disease (IBD) among first-, second-, and third-degree (FDR, SDR, TDR) among relatives of patients with rheumatoid arthritis (RA) compared to the population. [Orange circle, p < 0.01]
Figure. Risk of autoimmune thyroiditis (AITD), celiac, systemic lupus erythematosus (SLE), and inflammatory bowel disease (IBD) among first-, second-, and third-degree (FDR, SDR, TDR) among relatives of patients with rheumatoid arthritis (RA) compared to the population. [Orange circle, p < 0.01]
To cite this abstract in AMA style:
Liao K, Seyok T, Cannon-Albright L. Risk of Other Autoimmune Conditions Among Relatives of Patients with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/risk-of-other-autoimmune-conditions-among-relatives-of-patients-with-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-of-other-autoimmune-conditions-among-relatives-of-patients-with-rheumatoid-arthritis/
