Session Information
Date: Monday, November 8, 2021
Title: Systemic Sclerosis & Related Disorders – Clinical Poster II (1364–1390)
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: The clinical course of interstitial lung disease (ILD) in systemic sclerosis (SSc) is highly variable. Some patients experience a progressive decline in lung function while others remain stable. SSc patients with ILD may be monitored for progression by high-resolution computed tomography (HRCT), pulmonary function studies (PFT), or both, to determine i) need for therapy, or ii) stability on therapy. However, the percent change in ILD over time that constitutes significant progression on HRCT remains unclear. Additionally, whether short-term change in ILD% is associated with an increased risk for long-term ILD progression (traditionally defined as a reduction in forced vital capacity (FVC) on PFT of ≥10% predicted from baseline) is unknown. Small increases in ILD% on short-term follow-up HRCT scans may not be easily recognized due to high interrater variability in grading of the severity and extent of ILD on serial HRCT. The purpose of this study is to evaluate whether rate of change in interstitial lung abnormalities measured by quantitative CT (QCT) associates with long-term ILD progression.
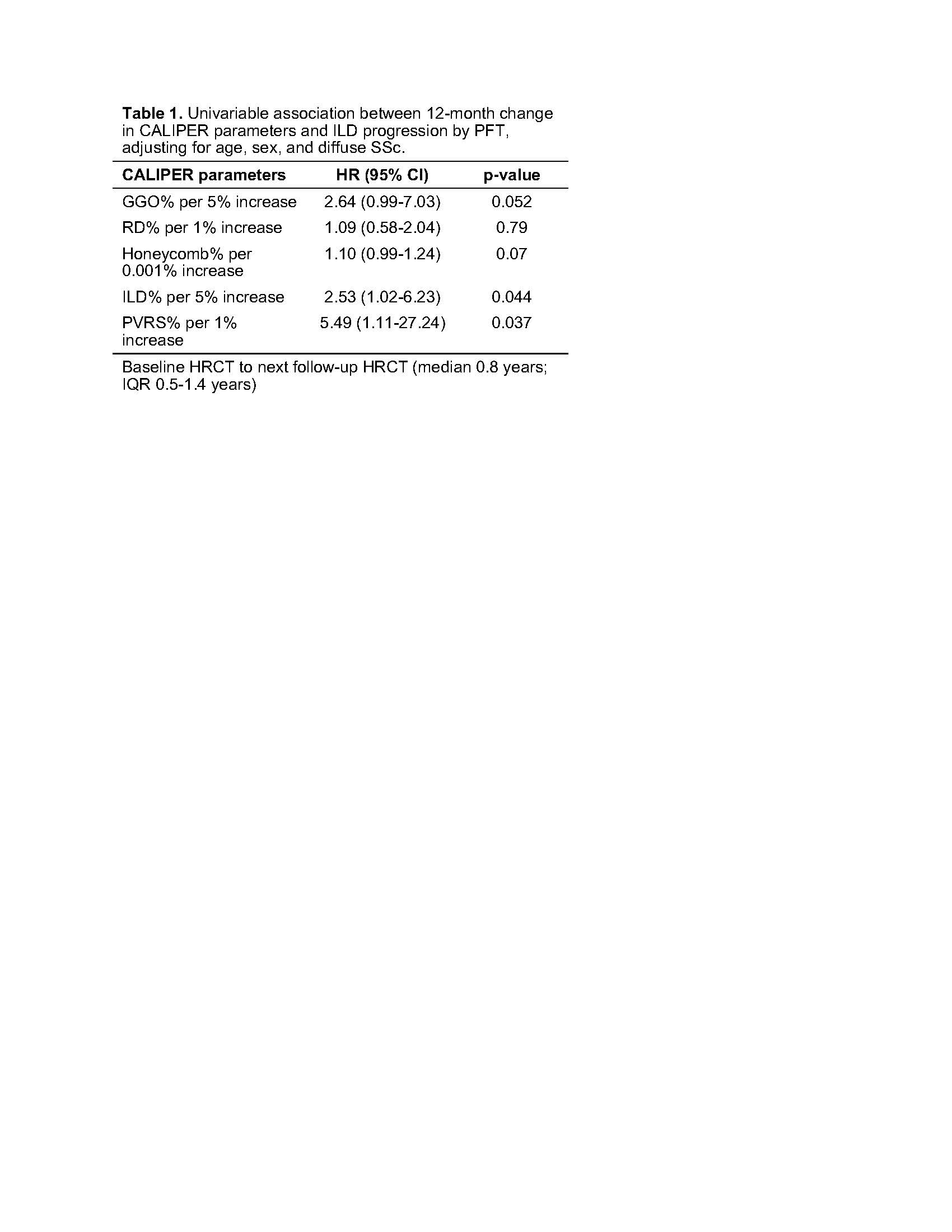
Methods: All patients meeting the 2013 ACR/EULAR Classification Criteria for SSc and seen between 2007 and 2019 at our institution were identified. Subjects were eligible for inclusion in this initial proof of concept study if they had a baseline HRCT ± 2 yrs of SSc diagnosis, a follow-up HRCT within 12 months ± 6 months of baseline HRCT, and had ≥5% total ILD on baseline HRCT. Additionally, subjects were required to have a baseline PFT ± 6 months of baseline HRCT, and at least one or more PFTs after the 12-month follow-up HRCT. Subjects were excluded if the eligible HRCT scans showed pulmonary edema secondary to heart failure, pleural effusions, malignancy, or infection. HRCTs were analyzed using CALIPER (Computed Aided Lung Informatics for Pathology Evaluation and Rating) QCT software, and all parenchymal (e.g. ground glass opacities (GGO), reticular densities (RD), honeycombing (HC)) and vascular features (pulmonary vascular related structures: PVRS) were quantified and normalized by total lung volume. Total ILD% is the summation of GGO%, RD%, and HC%. ILD progression was defined as a decline in FVC of ≥10% predicted from baseline PFT. The association between rate of change in quantitative parenchymal and vascular features and ILD progression was determined using Cox models.
Results: 36 subjects (75% female; mean age 60 yrs [SD 8.4]) were analyzed. Most had limited cutaneous SSc (75%) and had no current or prior history of smoking (69%). Median time under observation was 3.3 yrs (IQR 1.4, 4.6). A total of 8/34 subjects (24%) met ILD progression endpoint. A 5% increase in total ILD conferred a 2.5-fold increase in risk of ILD progression (HR: 2.53, 95% CI 1.02-6.23) (Table 1). A 1% increase in PVRS was associated with a 5-fold increase in risk of ILD progression (HR: 5.49, 95% CI 1.11-27.24).
Conclusion: QCT detects changes in parenchymal and vascular features on 1-year follow-up HRCT that may otherwise be too small to consistently detect and characterize by visual assessment, yet are early radiomic biomarkers of long-term disease progression risk. The utility of QCT in the evaluation and follow-up of SSc-ILD warrants further study.
To cite this abstract in AMA style:
Hinze A, Amin S, Makol A, Vassallo R, Crowson C, Bartholmai B. A 5% Increase in Interstitial Lung Disease at 1-Year Follow-up Is Associated with Long-Term ILD Progression in Systemic Sclerosis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/a-5-increase-in-interstitial-lung-disease-at-1-year-follow-up-is-associated-with-long-term-ild-progression-in-systemic-sclerosis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-5-increase-in-interstitial-lung-disease-at-1-year-follow-up-is-associated-with-long-term-ild-progression-in-systemic-sclerosis/