Session Information
Date: Sunday, November 7, 2021
Title: RA – Diagnosis, Manifestations, & Outcomes Poster II: Miscellaneous Aspects of RA (0786–0812)
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: Remission is a well-established optimal outcome in rheumatoid arthritis (RA) treatment, yet a minority of patients reach this goal. There is not one recognized definition for RA remission, but several sets of criteria regarded as remission or low disease activity. Except aggressive treatment and less time between diagnosis and treatment, little is known of what factors may impact RA remission. Building on a long-term collaboration of a non-profit organization and an academic rheumatology center, we explored factors associated with RA remission.
Methods: An anonymous survey was offered in 2019 on a secure online system. Participants were U.S. residents age ≥18 years with a self-reported RA diagnosis by a medical professional. They responded to questions on demographics, RA disease activity (DA), diagnosis and DMARD history, improvement from treatment, and RA treatment goals. Analyses included descriptive statistics with chi-square and rank sum tests for comparisons. Treatment goals were thematically coded and verified for reliability by a team using qualitative content analysis.
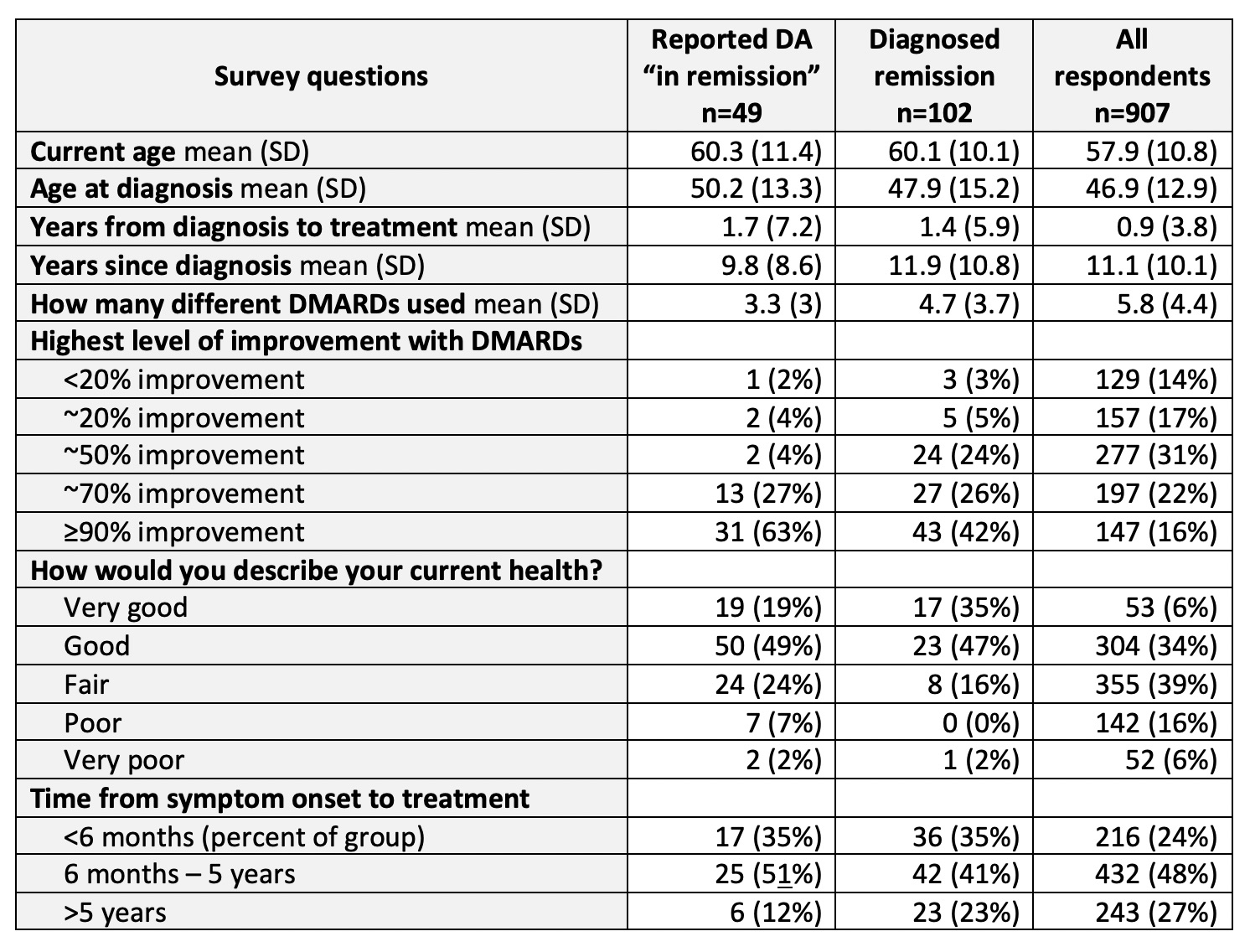
Results: The questionnaire was completed by 907 RA patients (90% women, 10% men), with 58 (11) mean (SD) years age and 11 (10) years since diagnosis. About twice as many reported being given an explicit diagnosis of RA remission (n=102; 11%) as patients who rated their DA as “in remission” (n=49; 5%). Patients rating their DA as in remission tried fewer different DMARDs than patients with more active disease (mean: remission 3.3; mild 4.2; moderate 5.7; severe DA 8.8). Those with diagnosed remission tried fewer mean DMARDs (4.7) than all respondents (5.8). Both self-reported remission and diagnosed remission were associated with less time between symptom onset and DMARD treatment. In both groups, about 35% were treated < 6 months of onset, but in all respondents, only 24% were treated this early. Both remission groups were associated with older current age and older age at diagnosis. Both remission groups were more likely to have had discussions with providers about RA treatment goals (diagnosed, 44% self-report, 51%) than all patients surveyed (37%).
Conclusion: This survey found previously unreported associations between remission and aspects of rheumatology care including time from symptom onset to treatment, age at diagnosis, and frequency of shared treatment goal discussions, independent of whether remission was clinically diagnosed or based on patient-reported DA levels. Our study is unique in that diagnosed remission is compared to self-reported DA “in remission,” the former being twice as frequent. Further research should seek greater insight on patient experiences in remission and explore how factors associated with remission may be used to increase the rate of remission in people with RA.
providers had discussed RA treatment goals with them.
To cite this abstract in AMA style:
O'Neill K, Marks K, Sinicrope P, Crowson C, Myasoedova E, Davis J. Relationships of Rheumatology Care and Patient Experiences to Rheumatoid Arthritis Remission [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/relationships-of-rheumatology-care-and-patient-experiences-to-rheumatoid-arthritis-remission/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/relationships-of-rheumatology-care-and-patient-experiences-to-rheumatoid-arthritis-remission/