Session Information
Date: Sunday, November 7, 2021
Title: Epidemiology & Public Health Poster II: Inflammatory Arthritis – RA, SpA, & Gout (0560–0593)
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: Higher comorbidity burden (CB) has been associated with treatment choices in RA, but not assessed in populations including multiple forms of inflammatory arthritis (IA) in routine practice settings. The Rheumatic Disease Comorbidity Index (RDCI), scored 0-9, is a validated method of quantifying CB in RA patients, but is infrequently reported in USA-based electronic health record (EHR)-derived cohort studies. The objective of this study is to examine if a higher CB is associated with differential prescribing and reported use (Rx) of oral glucocorticoids (GC) and TNF inhibitors (TNFi), therapies both commonly used to treat many forms of IA, using data from a new EHR-derived ‘Rheumatic and Arthritic Diseases Information Registry’ (RADIR) of patients with systemic rheumatic diseases (SRDs).
Methods: We constructed RADIR to include adults aged ≥ 18 years seen at least twice by a rheumatologist from 3/1/2018-2/28/2021 at a tertiary academic center in New York City. Eligible patients had ≥ 2 ICD-10-CM codes entered ≥7 days apart for a SRD which can present with IA. Patient data included demographics, labs, medications, and comorbid conditions (reported by ≥ 2 ICD-10-CM codes) to score the RDCI. Of 12,216 patients entered into RADIR, we included patients with forms of IA commonly treated with TNFi. IA patients included in this retrospective cohort study had ≥ 2 ICD-10-CM codes for RA, PsA, AS, SpA, JRA, JIA, Auto Inflammatory Syndromes, Enteric or Reactive Arthritis, Sarcoidosis, or Behcet’s Disease. Rx of GC and TNFi, demographics, and comorbidities were compared in IA patients with a low CB (RDCI ≤ 2) and high CB (RDCI > 2) by Pearson’s chi-squared tests. Two multivariable logistic regression models were used to assess for independent associations (odds ratio (OR), 95% CI) between RDCI score and Rx of GC and TNFi in IA, using age, gender, race, ethnicity, obese BMI and smoking as covariates.
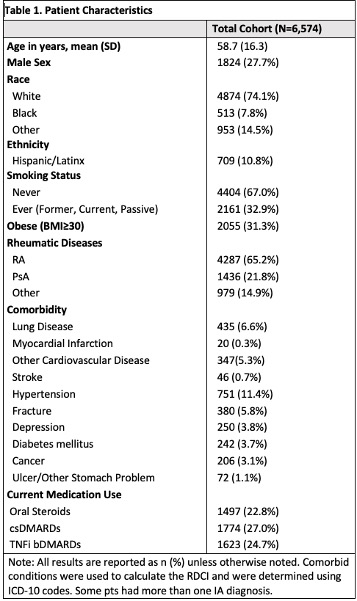
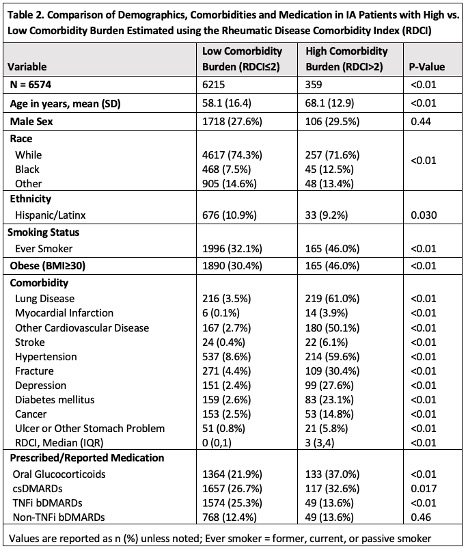
Results: Patients with 11 types of IA (n= 6,587) were mostly white (74%), female (72%), and without exposure to tobacco (67%) (Table 1). Most frequent forms of IA were RA (65%) and PSA (22%) (Table 1). Patients with a high CB (RDCI >2) were older and more often Black, Hispanic/Latinx, and with a BMI ≥ 30 (Table 2). Patients with a high CB had more Rx of GC and less Rx of TNFi (Table 2). Regression analyses revealed that for every 1 point increase in the RDCI, there was a 0.09 decrease in the odds of Rx of TNFi (OR 0.91, 95%CI [0.85, 0.98]) and a 0.26 increase in the odds (OR 1.26, 95%CI [1.19, 1.33]) of Rx of GC, while controlling for age, sex, race, ethnicity, obesity and smoking status (Table 3).
Conclusion: This analysis of a large sample of IA patients cared for in practice included in a new EHR-derived registry of SRDs indicates more patients will be prescribed GCs and fewer prescribed TNFi as CB progressively increases, a relationship previously only described in RA. These data suggest that IA patients with a high CB may be receiving suboptimal treatment. These findings may have implications regarding safety, effectiveness and health disparities of Rx patterns that warrant further investigation.
To cite this abstract in AMA style:
Rajesh D, Jannat-Khah D, Do H, Levine J, Barbhaiya M, Mandl L, Bykerk V. Comorbidity Burden as Scored Using the Rheumatic Disease Comorbidity Index (RDCI) Is Associated with Varying Treatment Patterns in Patients with Inflammatory Arthritis – a Study Using the EHR-Derived Rheumatic and Arthritis Disease Information Registry (RADIR) [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/comorbidity-burden-as-scored-using-the-rheumatic-disease-comorbidity-index-rdci-is-associated-with-varying-treatment-patterns-in-patients-with-inflammatory-arthritis-a-study-using-the-ehr/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/comorbidity-burden-as-scored-using-the-rheumatic-disease-comorbidity-index-rdci-is-associated-with-varying-treatment-patterns-in-patients-with-inflammatory-arthritis-a-study-using-the-ehr/