Session Information
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Intra-articular (IA) mineralization due to crystal deposition may contribute to OA pathology through inflammation, release of pro-catabolic factors, or altered cartilage biomechanical properties. Prior conflicting studies regarding whether chondrocalcinosis (from IA mineralization) is associated with OA structural progression were limited by the use of insensitive radiographs for visualizing IA mineralization. We studied the relation of IA mineralization on CT (a more sensitive modality) to cartilage loss on knee MRI in older adults, with particular attention to potential joint location- and tissue-specific effects of mineralization on cartilage pathology.
Methods: Participants from the Multicenter Osteoarthritis (MOST) study, a longitudinal prospective cohort of older adults, who had knee CTs and MRIs, were included in this longitudinal analysis. IA mineralization was assessed on CT using the Boston University Calcium Knee Score (BUCKS), with semi-quantitative scoring of extent of crystal mineralization 0-3 in WORMS subregions. We categorized presence of mineralization as a BUCKS score >0 in the following tissues: 1) anywhere in the knee; 2) cartilage; 3) meniscus; 4) joint capsule. For cartilage and meniscus, we further classified mineralization as occurring in the medial and/or lateral tibiofemoral compartment. Cartilage worsening on MRI was defined as any increase in the semi-quantitative MOAKS score between baseline and two-year follow-up in a compartment-specific manner and for the whole knee. We evaluated the relation of IA mineralization (defined above) to the presence of MRI cartilage worsening using binomial regression, and with generalized estimating equations for compartment-specific analyses to account for correlations between compartments within a knee. Analyses were performed in a compartment-specific manner for cartilage and meniscus mineralization (i.e., relation of presence of medial mineralization to risk of medial cartilage worsening), and at the whole knee level for capsular mineralization. Analyses were adjusted for age, sex, and body mass index (BMI).
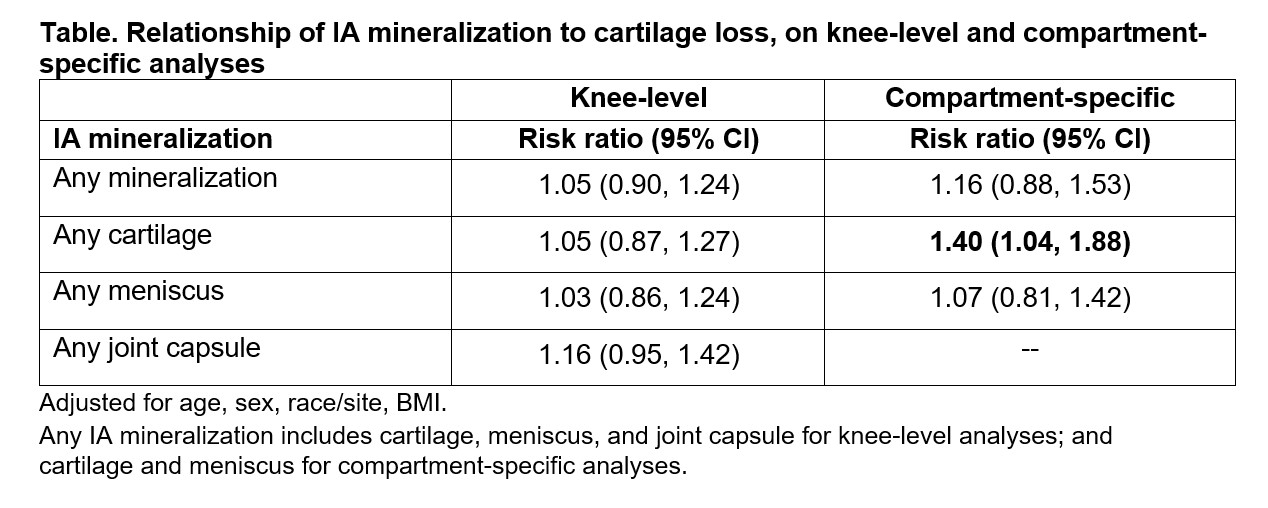
Results: We included 1673 participants (mean age 60.1±9.1, 56% female, mean BMI 28.6±5.0 kg/m2). Overall, 9.0% had any IA mineralization in the knee; mineralization in the cartilage, meniscus, and joint capsule was present in 6.3%, 7.1%, and 4.0%, respectively. 46.5% had cartilage loss on follow-up anywhere in the knee. In compartment-specific analyses, presence of cartilage mineralization was associated with a 1.40 higher risk of cartilage loss in the same compartment (95% CI, 1.04-1.88); no association was noted for mineralization of the meniscus (Table). Mineralization of any tissue in the knee, regardless of location or tissue type was not associated with cartilage worsening at any location in the knee.
Conclusion: IA mineralization in the cartilage, but not in the meniscus, was associated with higher risk of cartilage loss in the same compartment over two years. Mineralization of the joint capsule was also not associated with cartilage loss anywhere in the knee. These findings suggest potential tissue-specific and localized effects of IA mineralization on cartilage pathology in knee OA.
To cite this abstract in AMA style:
Liew J, Lynch J, Guermazi A, Jarraya M, Felson D, Wang N, Lewis C, Torner J, Nevitt M, Neogi T. Intra-Articular Mineralization on Knee CT and Risk of Cartilage Loss: The Multicenter Osteoarthritis Study [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/intra-articular-mineralization-on-knee-ct-and-risk-of-cartilage-loss-the-multicenter-osteoarthritis-study/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/intra-articular-mineralization-on-knee-ct-and-risk-of-cartilage-loss-the-multicenter-osteoarthritis-study/