Session Information
Date: Saturday, November 6, 2021
Title: Epidemiology & Public Health Poster I: COVID-19 & Vaccination (0084–0117)
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: New cases of the novel coronavirus disease (COVID-19) continue to occur even one year since the declaration of a global pandemic. Although most people will experience mild-to-moderate symptoms, some patients will experience severe and potentially fatal outcomes. Patients with rheumatic diseases may be at higher risk of experiencing severe outcomes compared to the general population. The purpose of this study was to compare the risk of hospitalization, admission to intensive care and mortality due to COVID-19 in patients with rheumatic diseases compared to the general population.
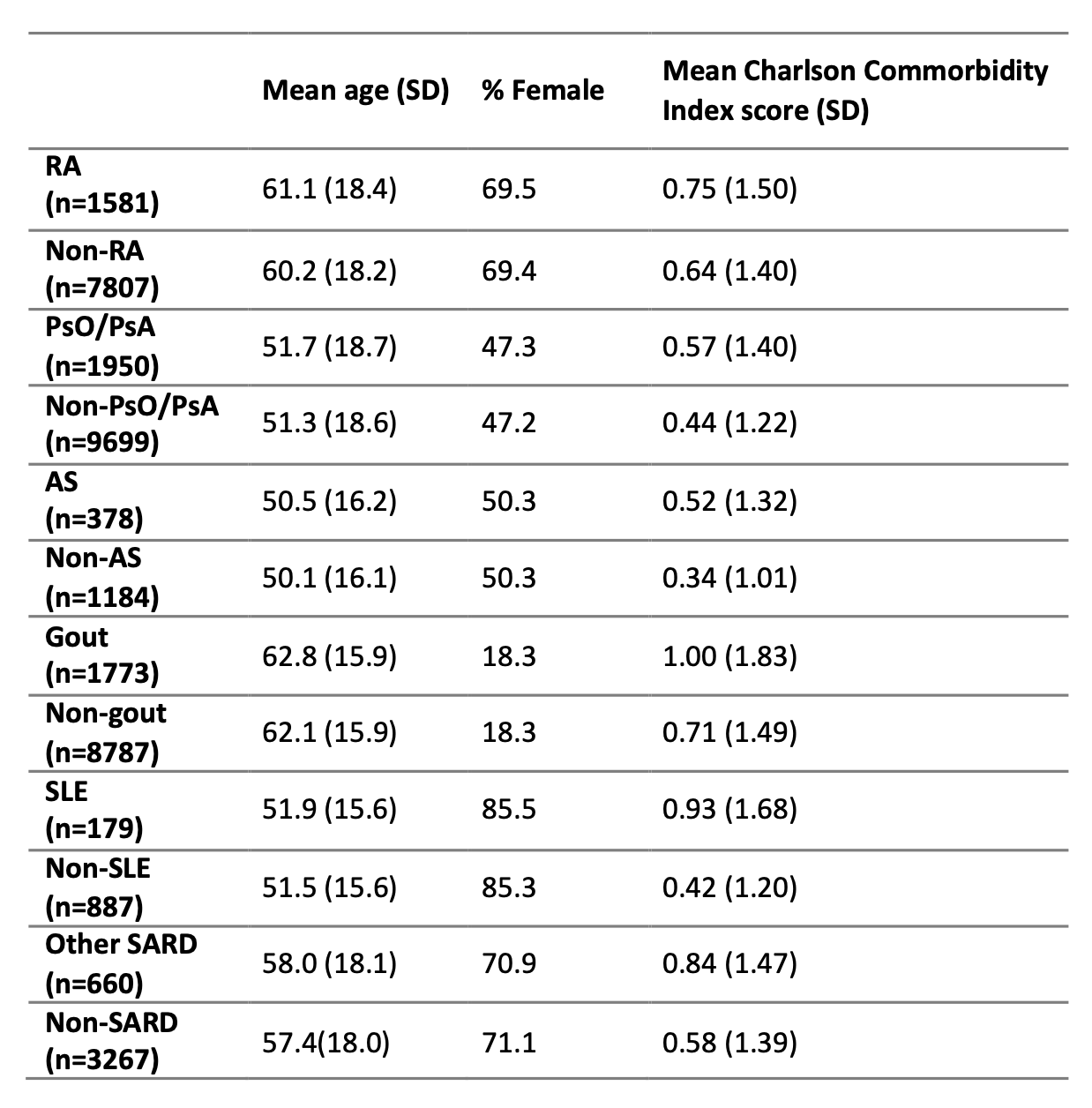
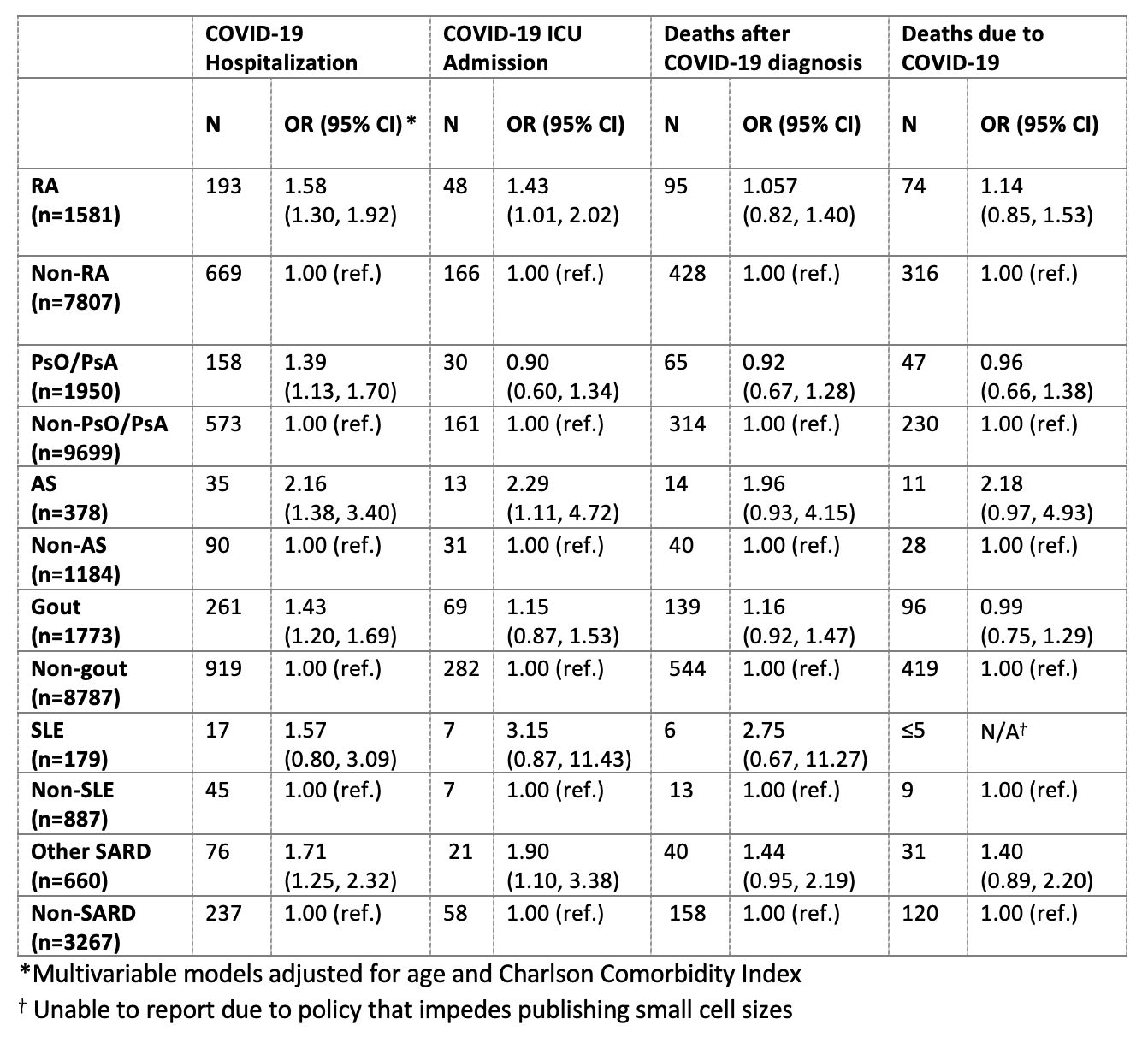
Methods: We used administrative health data from British Columbia (BC), Canada (population 5.1M) to conduct a population-based matched cohort study. Among all COVID-19 cases in BC between February 6, 2020 and April 15, 2021, we used ICD codes to identify all individuals with a rheumatic disease including: rheumatoid arthritis (RA), psoriasis/psoriatic arthritis (PsO/PsA), ankylosing spondylitis (AS), gout, systemic lupus erythematosus (SLE), and other systemic autoimmune rheumatic diseases (SARDs, including systemic sclerosis, Sjogren’s syndrome, myopathy, undifferentiated connective disease, and adult systemic vasculitides). All cases of COVID-19 were confirmed by a positive SARS-CoV-2 PCR test from the provincial Centre for Disease Control. Each individual with a rheumatic disease was matched with up to 5 individuals without rheumatic disease of similar age (± 5 years), sex, month and year of COVID-19 diagnosis and health authority. The risk of COVID-19 related hospitalization, intensive care unit (ICU) admission, mortality after COVID-19 diagnosis, and mortality with COVID-19 listed as primary cause were compared using multivariate logistic regression adjusting for age and Charlson Comorbidity Index score.
Results: Among the 104,508 cases of COVID-19 in BC up to April 15th, 2021, we matched 1581 individuals with RA, 1950 PsO/PsA, 378 AS, 1773 gout, 179 SLE, and 660 other SARDs to individuals without rheumatic disease. There was a statistically significant increase in the adjusted risk of hospitalization due to COVID-19 for individulas with RA (OR: 1.58),PsO/PsA (OR: 1.39), AS (OR: 2.16), gout (OR: 1.43), and other SARDs excluding SLE (OR: 1.71). While the risk of ICU admissions was significantly increased only for individuals with RA (OR: 1.43), AS (OR: 2.29) and other SARDs excluding SLE (OR: 1.90). Lastly, the risk of mortality was not significantly increased for individuals with rheumatic diseases compared to the general population.
Conclusion: Compared to individuals without a rheumatic disease, individuals with RA, PsO/PsA, AS, gout and SARDs excluding SLE were more likely to experience severe outcomes of COVID-19 including admissions to hospital and ICU. Furthermore, SLE was not associated with an increased risk of severe outcomes of COVID-19 when compared to the general population. Our findings have important implications for patients with certain rheumatic diseases and could inform targeted preventive measures, such as differential isolation measures, priority testing and optimization of vaccination schedules.
To cite this abstract in AMA style:
Avina-Galindo A, Marozoff S, Fazal Z, Kwan J, Lu N, Hoens A, Lacaille D, Kopec J, Xie H, Avina-Zubieta J. Risk of Hospitalization, Admission to Intensive Care and Mortality Due to COVID-19 in Patients with Rheumatic Diseases: A Population-based Matched Cohort Study [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/risk-of-hospitalization-admission-to-intensive-care-and-mortality-due-to-covid-19-in-patients-with-rheumatic-diseases-a-population-based-matched-cohort-study/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-of-hospitalization-admission-to-intensive-care-and-mortality-due-to-covid-19-in-patients-with-rheumatic-diseases-a-population-based-matched-cohort-study/