Session Information
Session Type: Abstract Session
Session Time: 10:00AM-10:50AM
Background/Purpose: Growing numbers of knee osteoarthritis (KOA) patients are morbidly obese (BMI ≥ 35 kg/m2). Evolving evidence suggests weight reduction may delay the structural progression of KOA, reduce knee pain, and improve total knee replacement (TKR) outcomes. The cost-effectiveness of surgical and non-surgical weight loss strategies among morbidly obese patients with KOA has not been assessed.
Methods: We used the Osteoarthritis Policy Model, a validated widely published microsimulation of KOA, to evaluate the cost-effectiveness of adding weight loss strategies to a KOA-related standard of care (SOC) in morbidly obese persons with KOA. The SOC includes physical therapy, NSAIDs, intra-articular injections, tramadol, oxycodone, TKR, and revision TKR. We considered 4 strategies: SOC only; SOC + a non-surgical weight loss (NSWL) program; SOC + Roux-en-Y Gastric Bypass (RYGB) surgery; and SOC + NSWL with RYGB after NSWL failure. For all strategies, we followed subjects until death, recording quality-adjusted life years (QALYs) accrued, lifetime medical costs, cumulative time in WOMAC pain states, and likelihoods of opioid and TKR use. We examined a KOA cohort with demographic and clinical characteristics consistent with those of patients enrolled in a long-term study of RYGB (mean age: 45, BMI: 46.6, WOMAC pain: 46.5). We used national databases and published data to estimate KOA structural progression, quality of life and background medical costs (stratified by pain, number of comorbidities, age, and BMI), treatment efficacy and costs ($14,819 for RYGB in year one and $251 in later years; $819 for NSWL in year one and $294 in later years), and costs and risks of complications. In sensitivity analyses we varied: the cost of health consequences of class III obesity (BMI ≥ 40) relative to class II (35 ≤ BMI < 40)($0 to $1,555 (base case = $1,555)), the likelihood of adverse events from RYGB (-50% to 50% relative to base case), and the maximum years weight loss from RYGB is maintained (5 to 20 (base case = 20)). We discounted costs and QALYs at 3%/year and conducted analysis from a healthcare perspective. We evaluated cost-effectiveness by calculating incremental cost-effectiveness ratios (ICERs) as the ratio of change in costs to change in QALYs for competing strategies in 2019 USD.
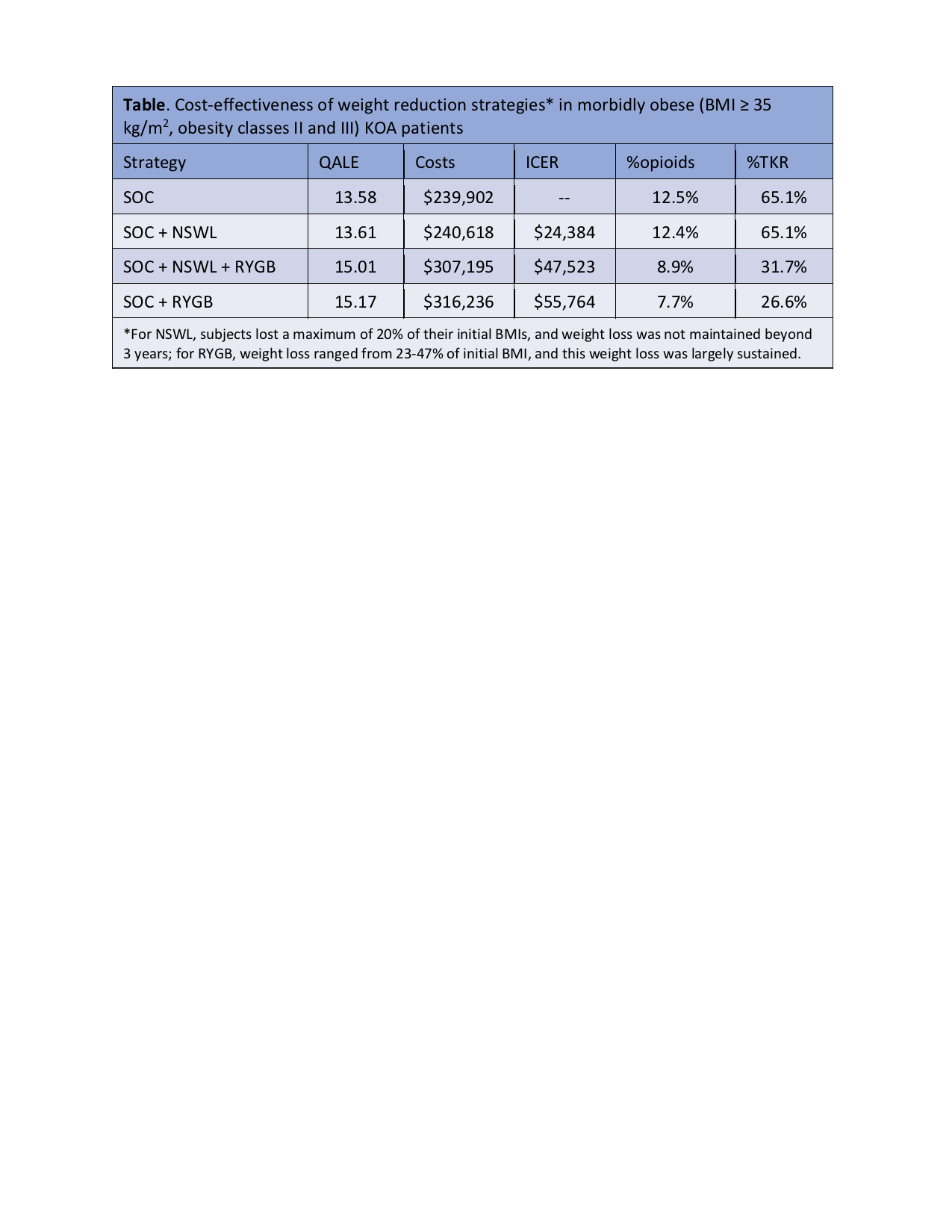
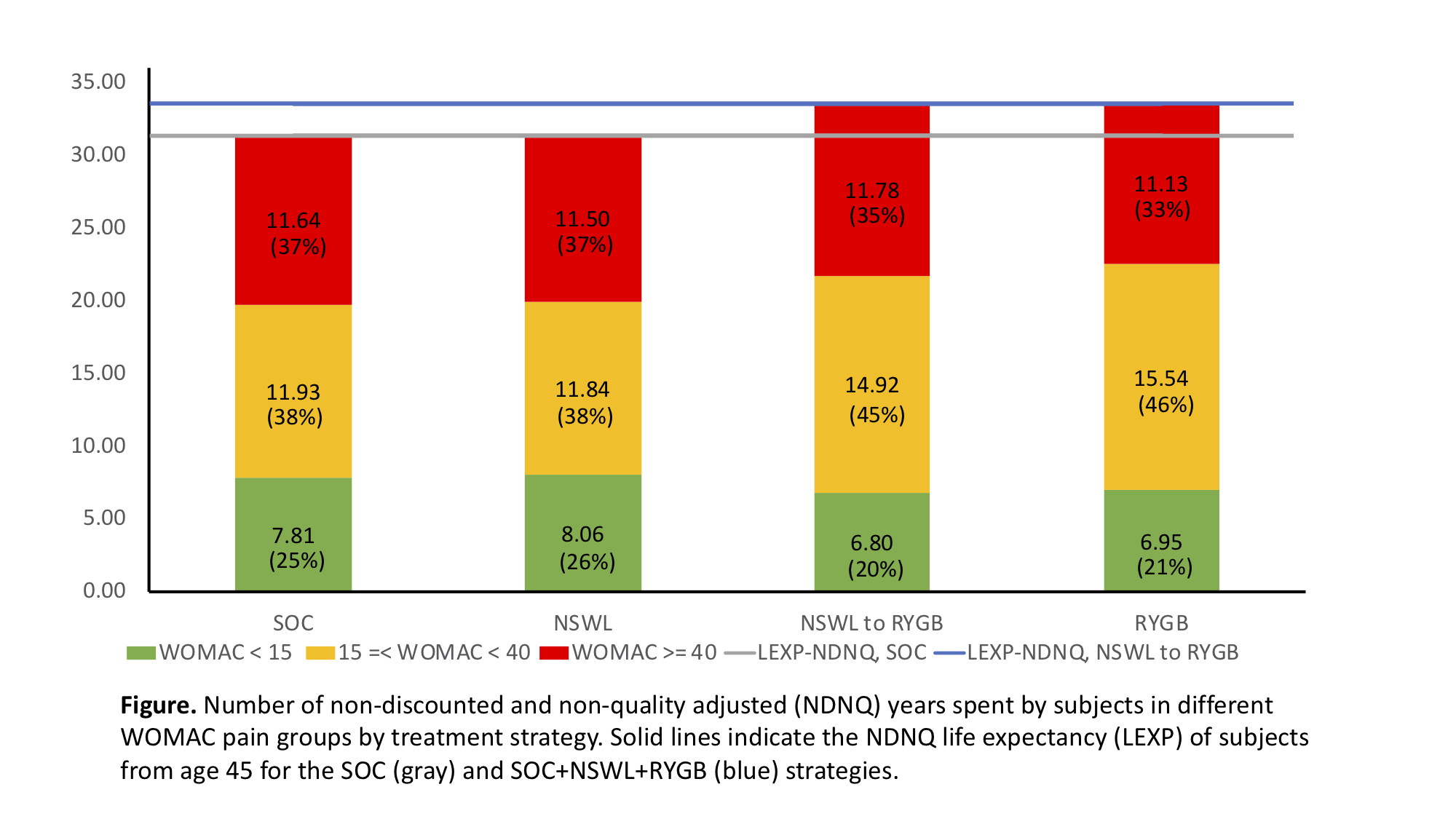
Results: Among morbidly obese patients with KOA, adding NSWL to the SOC added 0.3 QALYs and $716 in medical costs, resulting in an ICER of $24,384. Relative to the SOC + NSWL strategy, adding RYGB after NSWL added 1.4 QALYs and $66,577 in costs, leading to an ICER of $47,523. Relative to NSWL + RYGB, RYGB alone added 0.16 QALYs and $9,041 in costs with an ICER of $55,764. Relative to the SOC, the RYGB alone and NSWL + RYGB strategies reduced opioid use from 12.5% to 7.7-8.9%, and TKR use from 65.1% to 27-32% (Table). Number of years spent in different WOMAC pain groups are reported for each strategy (Figure). In sensitivity analyses, the additional cost of class III obesity was the most influential parameter affecting the cost-effectiveness of RYGB.
Conclusion: RYGB is cost-effective when preceded by NSWL at a willingness to pay (WTP) threshold of $50K/QALY. Proceeding directly to RYGB is cost-effective at a WTP threshold of $60K/QALY or higher.
To cite this abstract in AMA style:
Leifer V, Katz J, Selzer F, Neogi T, Collins J, Losina E. Cost-effectiveness of Surgical and Non-Surgical Weight Loss Programs for Morbidly Obese Patients with Knee Osteoarthritis [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/cost-effectiveness-of-surgical-and-non-surgical-weight-loss-programs-for-morbidly-obese-patients-with-knee-osteoarthritis/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/cost-effectiveness-of-surgical-and-non-surgical-weight-loss-programs-for-morbidly-obese-patients-with-knee-osteoarthritis/