Session Information
Date: Monday, November 9, 2020
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: In rheumatic and musculoskeletal diseases, physician global assessment (PhGA) is a major factor of treatment decision. However, it is not well-known which disease manifestations contribute to PhGA in early axSpA and if contextual factors have an impact. The objective of this study is to investigate determinants of PhGA and the influence of contextual factors on this relationship in patients with early axSpA.
Methods: Five-year data from DESIR, a cohort of early axSpA, were analysed. Clinical data were collected every 6 months up to 2 years and annually thereafter. The primary analysis included all patients, and the subgroup analysis patients with follow-up MRI at 2 and/or 5 years. PhGA over 5 years was the outcome of interest. Univariable generalized estimating equation (GEE) models were used to investigate relationships between potential determinants and PhGA. Longitudinal relationships were investigated in autoregressive models. Effect modification by contextual factors (educational level, gender and age) was tested and, if significant, models were stratified. Univariable analyses were chosen to better assess the contributory explanatory effects of each of the determinants in each of the strata.
Results: A total of 708 patients were included, mean age 33.7 (SD 8.6) years, 46% male, 41% lower educated. The subgroup consisted of 220 patients with similar characteristics. Higher BASDAI questions 1-6, SJC28, TJC53, Maastricht Ankylosing Spondylitis Enthesitis Score (MASES), CRP and BASMI were associated with a higher PhGA (Table 1). Gender and age were effect modifiers of SJC28; the effect was largest in the younger male stratum (β [95% CI]; 1.07 [0.71, 1.43] ), and smallest in the older female stratum (0.13 [0.04, 0.22]) (Figure 1). Autoregressive GEE models revealed the same determinants of PhGA and the same pattern of effect by gender and age.
Conclusion: Patient’s subjective symptoms, peripheral arthritis, enthesitis, higher CRP and impaired spinal mobility contribute to explain PhGA in patients with early axSpA irrespective of gender and age. But physicians consider the presence of swollen joints as more important in males than in females.
 Table 1. Factors associated with PhGA over time in gender/age-stratified groups in univariable analysis
Table 1. Factors associated with PhGA over time in gender/age-stratified groups in univariable analysis
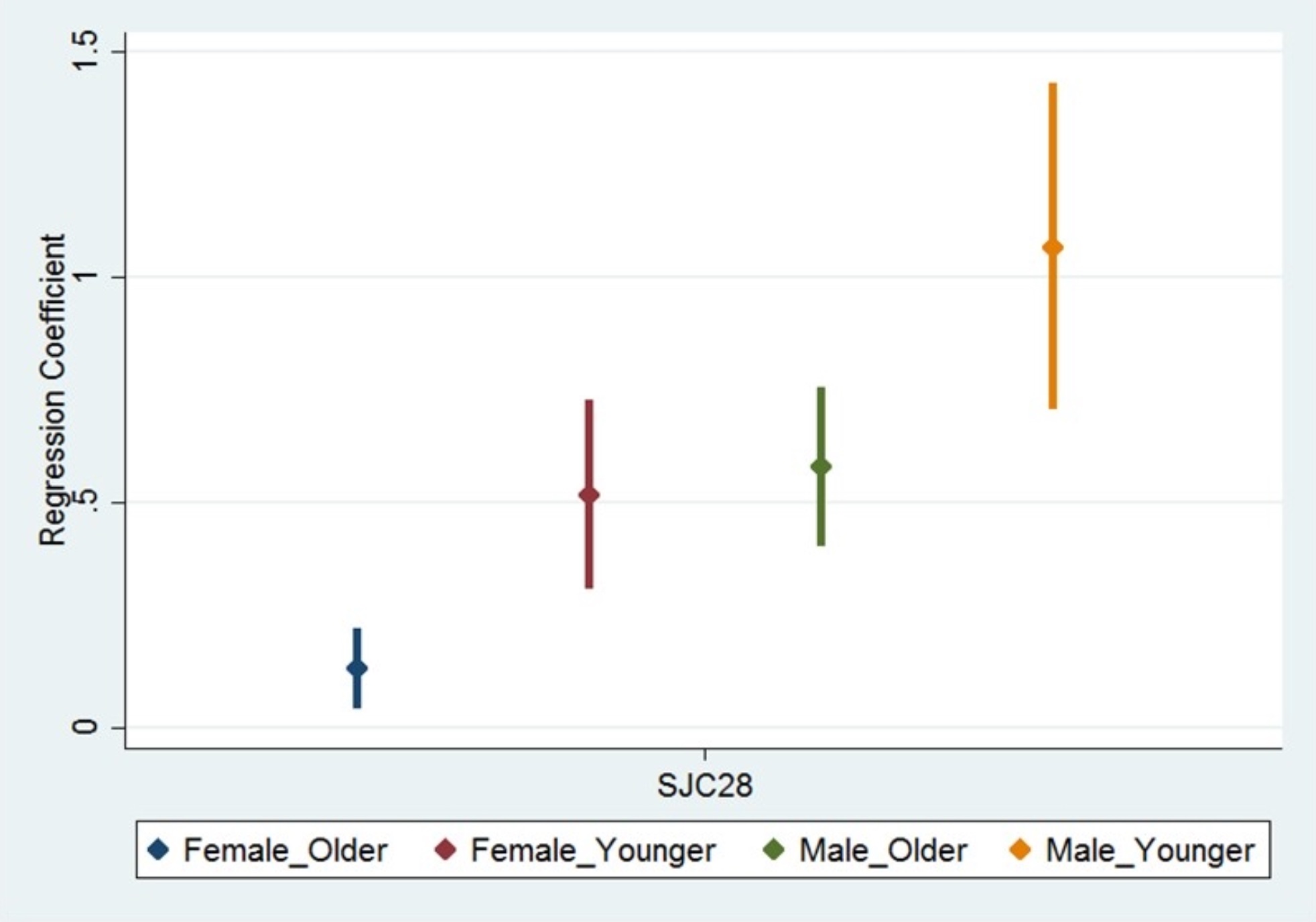 Figure 1. Impact of swollen joint count on physician global assessment across gender and age groups. Regression coefficients (95% CI) of the effect of SJC28 on PhGA in the univariable GEE analyses across gender/age-stratified groups (in an ascending order).
Figure 1. Impact of swollen joint count on physician global assessment across gender and age groups. Regression coefficients (95% CI) of the effect of SJC28 on PhGA in the univariable GEE analyses across gender/age-stratified groups (in an ascending order).
To cite this abstract in AMA style:
Hirano F, Landewé R, van Gaalen F, van der Heijde D, Gaujoux-Viala C, Ramiro S. Determinants of Physician Global Assessment and Influence of Contextual Factors in Early Axial Spondyloarthritis [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/determinants-of-physician-global-assessment-and-influence-of-contextual-factors-in-early-axial-spondyloarthritis/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/determinants-of-physician-global-assessment-and-influence-of-contextual-factors-in-early-axial-spondyloarthritis/
