Session Information
Date: Monday, November 9, 2020
Title: Pediatric Rheumatology – Clinical Poster III: SLE, Vasculitis, & JDM
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: Renal involvement in childhood-onset systemic lupus erythematosus (cSLE) is a major cause of morbidity and mortality. Current tools to identify lupus nephritis (LN) fall short compared to renal biopsy. The renal activity index in lupus (RAIL) was developed using 6 urinary biomarkers to reflect disease activity(1).
Purpose: To test the usefulness of the RAIL in the clinical setting to identify children with active LN.
Methods: Urine samples were collected cross-sectionally from cSLE patients at the time of active LN or routine clinic visit. Patients were classified into active LN, inactive LN or non-LN SLE based on results of a renal biopsy and/or absence of LN determined by routine urinalysis. The following urine biomarkers are included in the RAIL score (neutrophil gelatinase-associated lipocalin, ceruloplasmin, monocyte chemoattractant protein-1, adiponectin, hemopexin, kidney injury molecule-1, urinary protein and creatinine). Analysis was done by Enzyme-linked immunosorbent assay (ELISA) and nephelometry. RAIL scores were calculated per the defined algorithm. The accuracy of the RAIL score was compared between groups.
Results: Among 117 cSLE patients, 37 had active LN, 30 had inactive LN and 50 had no LN. Clinical characteristics and distribution of RAIL scores are outlined in Table 1. RAIL scores of inactive LN and no-LN group largely overlapped so they were combined in one group (Group 2) and compared to active LN (Group 1). The RAIL score was significantly higher in Group 1 vs Group 2 (median 0.7 vs -1.1 respectively, p< 0.0001). The RAIL score diagnostic accuracy was assessed in a multivariable regression model. Adjusting for patient’s age and extra-renal SLE activity index (SLEDAI) score, the RAIL score was associated with odds ratio of 2.16 (95%CI 1.4-3.3, p=0.001) for active LN vs. inactive LN and non-LN SLE. A receiver operating curve for a RAIL cut-off score of 0.35 produced an area under the curve of 0.9 (sensitivity 86%, specificity 84%) for active LN. A RAIL score < 0.35 had a negative likelihood ratio of 0.17. Further adjustment for urinary protein and creatinine did not significantly influence the results.
Conclusion: The RAIL score is highly accurate in distinguishing active LN identified by renal biopsy, from inactive LN and non-LN SLE. A score of 0.35 identifies cSLE patients who very likely have active LN.
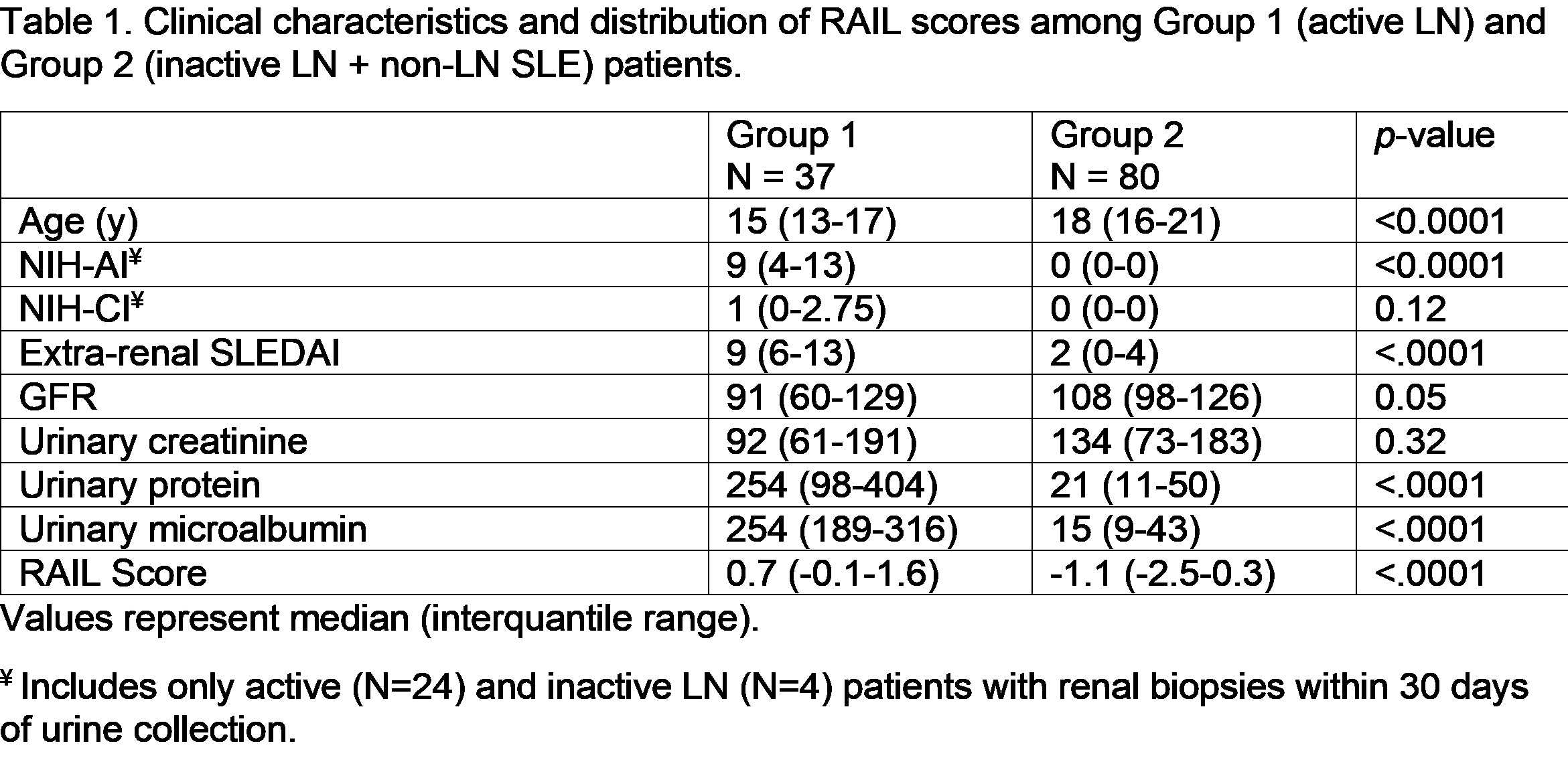 Table 1. Clinical characteristics and distribution of RAIL scores among Group 1 (active LN) and Group 2 (inactive LN + non-LN SLE) patients.
Table 1. Clinical characteristics and distribution of RAIL scores among Group 1 (active LN) and Group 2 (inactive LN + non-LN SLE) patients.
 Figure 1. Receiver Operating Curve (ROC) for the RAIL score in differentiating active LN (Group 1) from Inactive LN & non-LN SLE (Group 2).
Figure 1. Receiver Operating Curve (ROC) for the RAIL score in differentiating active LN (Group 1) from Inactive LN & non-LN SLE (Group 2).
To cite this abstract in AMA style:
Aljaberi N, Mathur A, Jose S, Hennard T, Merritt A, Ma Q, Rose J, Sahay R, Liu C, Wenderfer S, Brunner H. Renal Activity Index for Lupus Nephritis Distinguishes Active Renal Disease Among Childhood Systemic Lupus Erythematosus Patients [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/renal-activity-index-for-lupus-nephritis-distinguishes-active-renal-disease-among-childhood-systemic-lupus-erythematosus-patients/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/renal-activity-index-for-lupus-nephritis-distinguishes-active-renal-disease-among-childhood-systemic-lupus-erythematosus-patients/
