Session Information
Date: Sunday, November 8, 2020
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Few studies have investigated the overall occurrence of comorbidities in patients with non-radiographic axial spondyloarthritis (nr-axSpA) in relation to ankylosing spondylitis (AS). Compared to nr-axSpA, AS patients are generally older and display higher inflammatory markers in blood, both known risk factors of comorbidity. The Charlson Comorbidity Index (CCI) is a commonly used instrument to assess comorbidity. Originally designed to predict mortality, the CCI assigns weighted points for both comorbidities and age, but can also be used without age-points.[1] The purpose of this study was to compare comorbidity burden between well-characterized patients with nr-axSpA and AS.
Methods: Patients with clinical axial spondyloarthritis diagnoses, consecutively enrolled in a population-based, cross-sectional cohort study, were thoroughly examined and classified as nr-axSpA (ASAS criteria; n=86) or AS (modified New York criteria; n=168). CCI scores without age-points were calculated from patient-reported data and compared between the nr-axSpA and AS groups. Age-points were omitted since we aimed to assess current comorbidity burden, rather than to predict mortality. A corresponding comparison was also conducted regarding the number of CCI associated comorbidities (comorbidity count; n=0-13, without weighted points) reported by each patient. Analyses were performed by linear regression, unadjusted as well as adjusted for age, sex, level of education (proxy for socioeconomic status), smoking, alcohol habits and body mass index. Due to the skewed distribution of CCI scores and comorbidity counts, confidence intervals were calculated by non-parametric bootstrapping with 10,000 iterations. Additionally, the proportion of patients in each group reporting ≥1 comorbidity (as defined by CCI) was compared by logistic regression, unadjusted and adjusted for age (further adjustment not possible due to few events).
Results: Patient characteristics for the nr-axSpA and AS groups are shown in Table 1. Compared to the AS group, nr-axSpA patients were younger and a greater proportion were women. Both groups showed a relatively small total number of comorbidities, and the occurrence of the individual comorbidities did not differ between the groups (Table 2). In unadjusted analyses, CCI without age-points, as well as comorbidity count, were not significantly different between the groups (Figure). However after adjustment for the younger age of the nr-axSpA patients, both CCI without age-points and comorbidity count were found to be significantly higher in the nr-axSpA group, and remained so also in the fully adjusted analyses (Figure). Finally, comparing the proportion of patients having ≥1 comorbidity produced analogous results (Figure).
Conclusion: Our results indicate that in a population-based, cross-sectional setting the burden of serious comorbidities, as assessed by CCI, is at least as high in patients with nr-axSpA as in AS. Despite the well-described lower systemic inflammation in patients with nr-axSpA, our results thus suggest that medical vigilance to target and prevent comorbidities in this group is equally important as in AS.
Reference:
1. Charlson ME, et al. J Chron Dis. 1987;40:373-83.
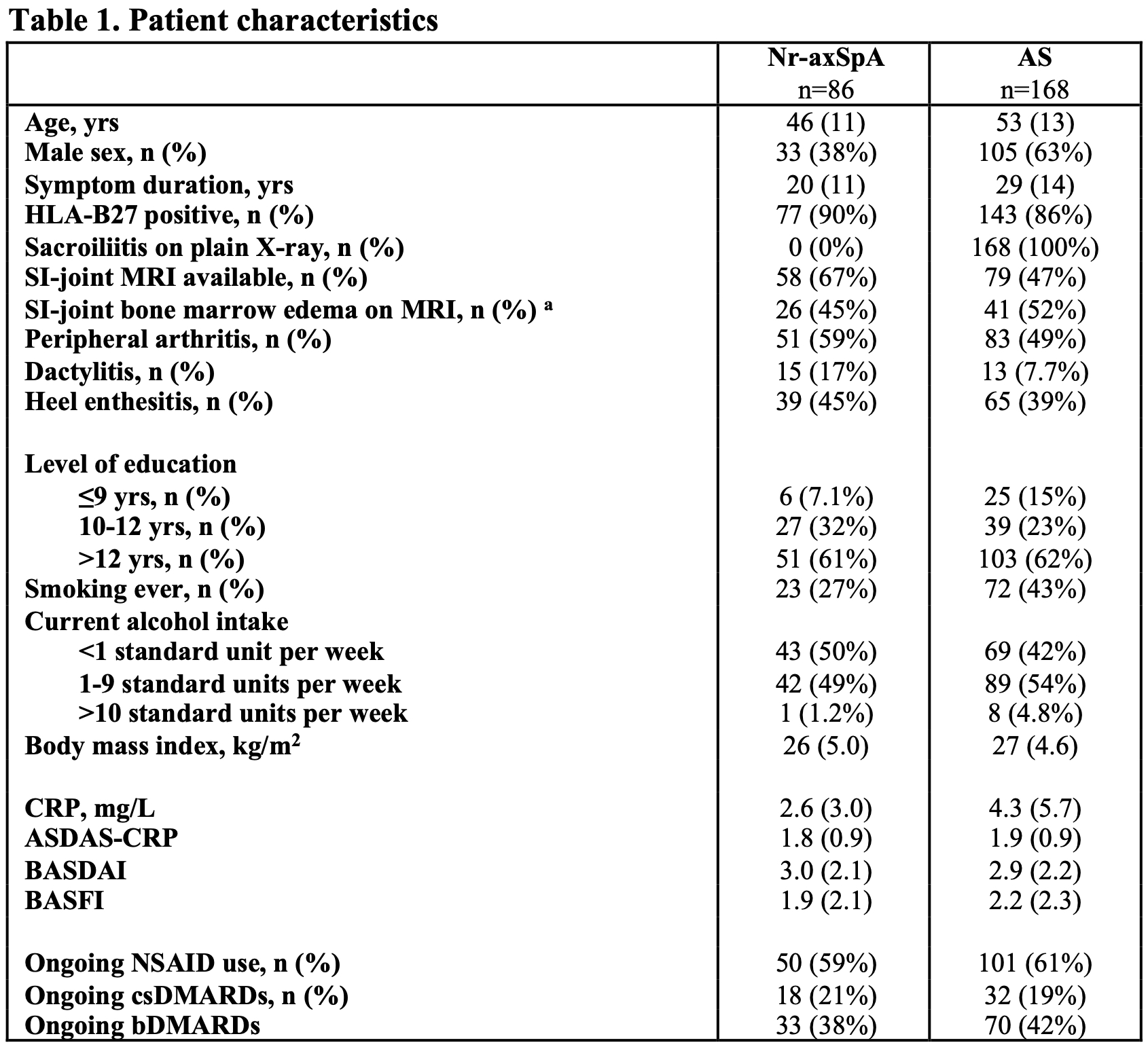 Mean (SD) if not stated otherwise. a Previous or current SI-joint bone marrow edema according to the ASAS definition. Missing data, n (%): Symptom duration 2 (0.8%); HLA-B27 1 (0.4%); Level of education 3 (1.2%); Current alcohol intake 2 (0.8%); CRP 29 (11%); ASDAS-CRP 35 (14%); BASDAI 17 (6.7%); BASFI 19 (7.5%); NSAID use 3 (1.2%). ASAS, Asessment of SponyloArthritis international Society; ASDAS-CRP, ankylosing spondylitis disease activity score using CRP; BASDAI, Bath ankylosing spondylitis disease activity index; BASFI, Bath ankylosing spondylitis functional index; bDMARD, biologic disease-modifying anti-rheumatic drug; CRP, C-reactive protein; csDMARD, conventional synthetic disease-modifying anti-rheumatic drug; HLA, human leukocyte antigen; MRI, magnetic resonance imaging; yrs, years; NSAID, non-steroidal anti-inflammatory drug; SD, standard deviation; SI, sacroiliac.
Mean (SD) if not stated otherwise. a Previous or current SI-joint bone marrow edema according to the ASAS definition. Missing data, n (%): Symptom duration 2 (0.8%); HLA-B27 1 (0.4%); Level of education 3 (1.2%); Current alcohol intake 2 (0.8%); CRP 29 (11%); ASDAS-CRP 35 (14%); BASDAI 17 (6.7%); BASFI 19 (7.5%); NSAID use 3 (1.2%). ASAS, Asessment of SponyloArthritis international Society; ASDAS-CRP, ankylosing spondylitis disease activity score using CRP; BASDAI, Bath ankylosing spondylitis disease activity index; BASFI, Bath ankylosing spondylitis functional index; bDMARD, biologic disease-modifying anti-rheumatic drug; CRP, C-reactive protein; csDMARD, conventional synthetic disease-modifying anti-rheumatic drug; HLA, human leukocyte antigen; MRI, magnetic resonance imaging; yrs, years; NSAID, non-steroidal anti-inflammatory drug; SD, standard deviation; SI, sacroiliac.
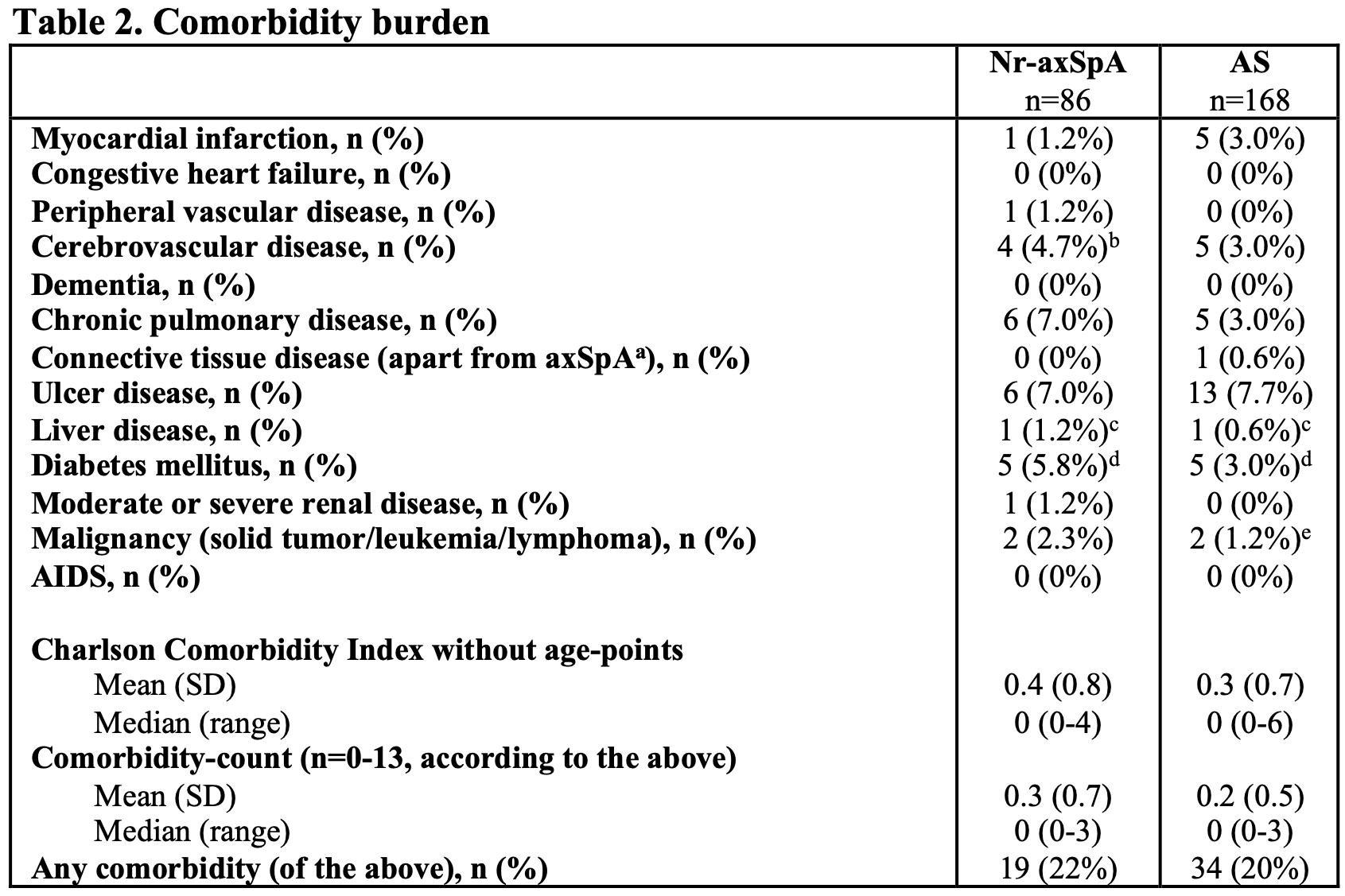 No significant between-group difference in any of the individual comorbidities by Chi2-test / Fisher´s Exact Test, as appropriate. a Systemic lupus erythematous, polymyositis, mixed connective tissue disease, polymyalgia rheumatica or moderate to severe rheumatoid arthritis. b One nr-axSpA patient with hemiplegia. c None with moderate or severe liver disease. d Two AS and one nr-axSpA patient with end organ damage. e One AS patient with metastatic solid tumor. Nr-axSpA, non-radiographic axial spondyloarthritis; AS, ankylosing spondylitis; axSpA, axial spondyloarthritis; SD, standard deviation.
No significant between-group difference in any of the individual comorbidities by Chi2-test / Fisher´s Exact Test, as appropriate. a Systemic lupus erythematous, polymyositis, mixed connective tissue disease, polymyalgia rheumatica or moderate to severe rheumatoid arthritis. b One nr-axSpA patient with hemiplegia. c None with moderate or severe liver disease. d Two AS and one nr-axSpA patient with end organ damage. e One AS patient with metastatic solid tumor. Nr-axSpA, non-radiographic axial spondyloarthritis; AS, ankylosing spondylitis; axSpA, axial spondyloarthritis; SD, standard deviation.
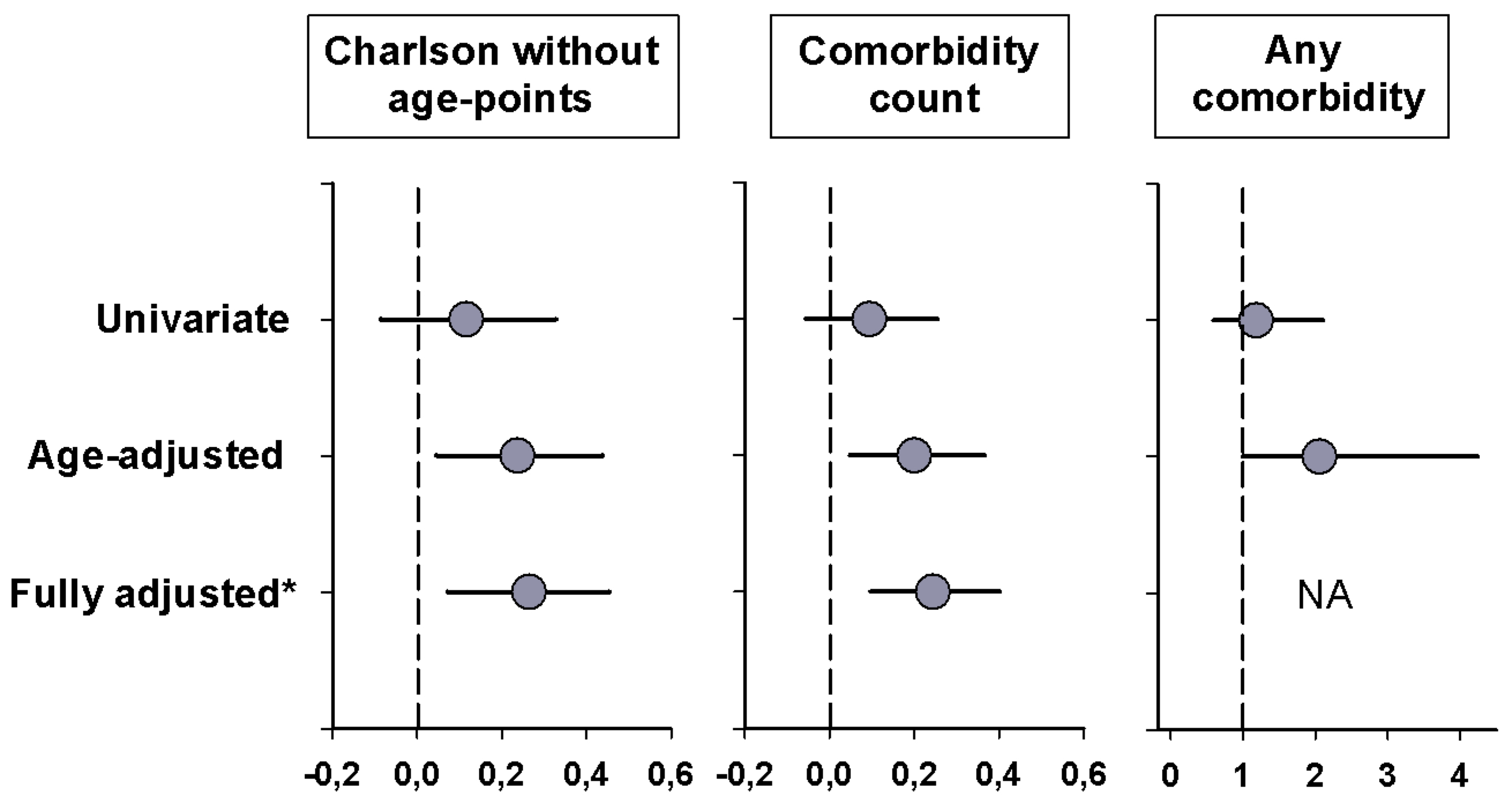 Figure. Differences between patients with nr-axSpA and AS (reference) regarding Charlson comorbidity index without age-points (left panel), comorbidity count (middle panel), and presence of any comorbidity (right panel). For the left and middle panels, data shown represent point estimate differences (dots) with 95% CI (whiskers) from unadjusted analyses, analyses adjusted only for age, and fully adjusted analyses (* adjustment for age, sex, education level, smoking, alcohol habits and body mass index). For the right panel, data shown represent odds ratios (dots) with 95% CI (whiskers) from unadjusted and age-adjusted analyses, respectively (further adjustment not possible due to too few events). NA, non-applicable.
Figure. Differences between patients with nr-axSpA and AS (reference) regarding Charlson comorbidity index without age-points (left panel), comorbidity count (middle panel), and presence of any comorbidity (right panel). For the left and middle panels, data shown represent point estimate differences (dots) with 95% CI (whiskers) from unadjusted analyses, analyses adjusted only for age, and fully adjusted analyses (* adjustment for age, sex, education level, smoking, alcohol habits and body mass index). For the right panel, data shown represent odds ratios (dots) with 95% CI (whiskers) from unadjusted and age-adjusted analyses, respectively (further adjustment not possible due to too few events). NA, non-applicable.
To cite this abstract in AMA style:
Sagard J, Lindqvist E, Mogard E, Jöud A, Geijer M, Olofsson T, K. Wallman J. Comorbidity Burden in Patients with Non-Radiographic Axial Spondyloarthritis at Least as High as in Ankylosing Spondylitis [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/comorbidity-burden-in-patients-with-non-radiographic-axial-spondyloarthritis-at-least-as-high-as-in-ankylosing-spondylitis/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/comorbidity-burden-in-patients-with-non-radiographic-axial-spondyloarthritis-at-least-as-high-as-in-ankylosing-spondylitis/
