Session Information
Date: Sunday, November 8, 2020
Title: Pediatric Rheumatology – Clinical Poster II: Systemic JIA, Autoinflammatory, & Scleroderma
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Localized scleroderma (LS) is a rare, progressive autoimmune disease of the skin and underlying connective tissue that can result in devastating functional impairment and cosmetic damage in children. Approximately 25% of patients with pediatric-onset LS have the craniofacial (Cf-LS) subtype, with scalp and face involvement known as en coup de sabre or Parry Romberg Syndrome. Standardized cutaneous evaluations may be limited for monitoring craniofacial lesions due to deeper tissue involvement. Advanced stereophotogrammetrical imagers create high-resolution 3D craniofacial models that can be manipulated and analyzed to identify degree and location of facial asymmetry, such as seen in Cf-LS. Normative measurements of asymmetry have been suggested. (Taylor HO, et al. Quantitative facial asymmetry: using three-dimensional photogrammetry to measure baseline facial surface symmetry. J Craniofac Surg. 2014;25(1):124-128)
Our goal was to longitudinally assess patients with Cf-LS to determine the course of facial asymmetry over time. We hypothesize that patients with Cf-LS have facial asymmetry beyond normative data which is maintained that can reliably be detected and tracked longitudinally via computerized stereophotogrammetrical measurements.
Methods: Patients (N=5) with craniofacial scleroderma (en coup de sabre and/or Parry Romberg Syndrome) were retrospectively identified in the National Registry for Childhood Onset Scleroderma (NRCOS). Demographic data, medication use, and standardized cutaneous outcomes were extracted from the NRCOS database. This data was paired with clinical 3D facial maps collected via Canfield VECTRA M3 or 3dMD.head.t imaging systems. Image surfaces were analyzed in Vectra Analysis Module. Trimmed and registered images were divided along the plane of maximal symmetry utilizing VAM automated alignment. The hemi-face was then reflected about this plane to superimpose the affected and unaffected sides. Root mean square deviation (RMSD) in millimeters was calculated for each reflection as the main outcome measure. Descriptive statistics were applied.
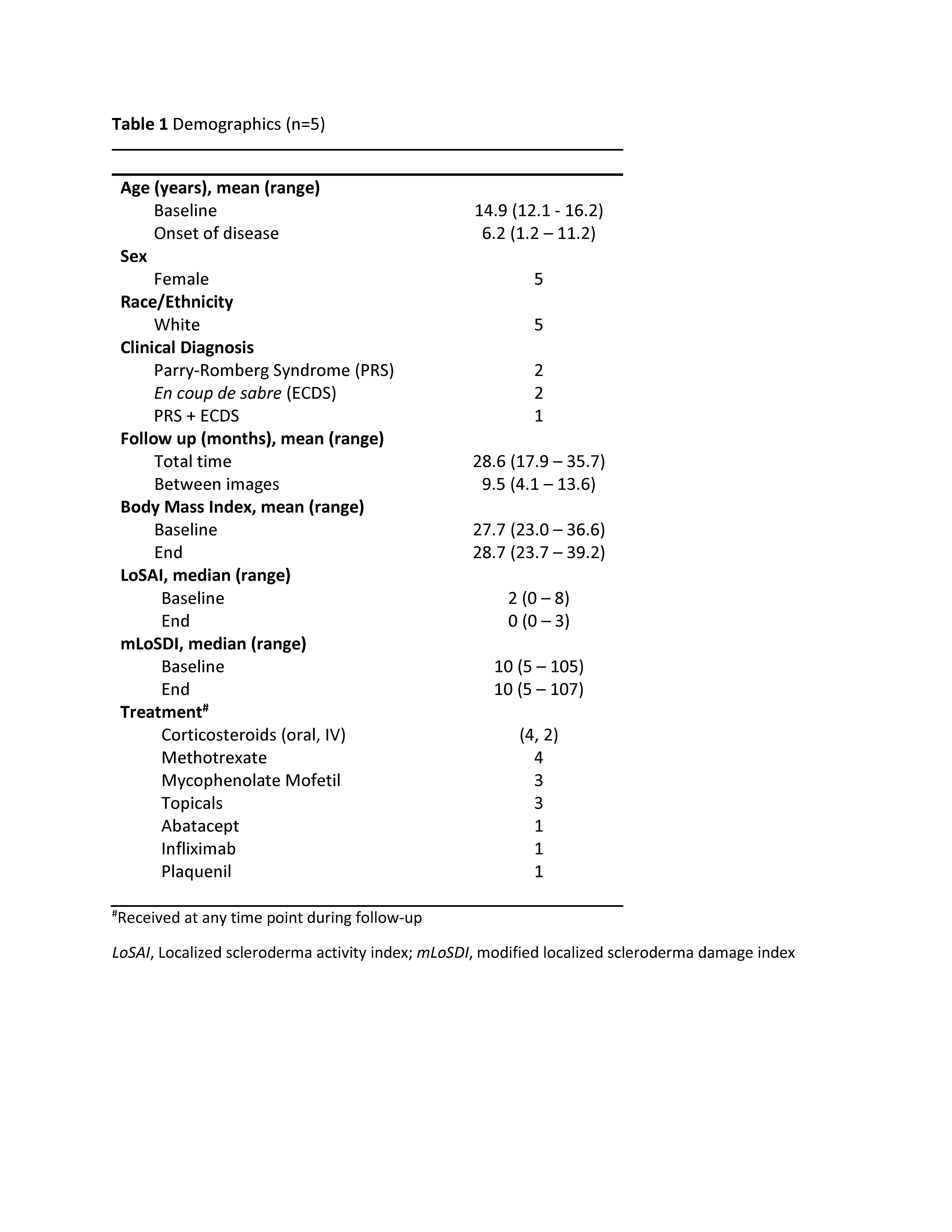
Results: Patients were followed for a mean of 28.6 months (Table 1). Body-mass index (BMI) was relatively stable across the follow up period. All patients received systemic immunomodulation during the follow-up period. Standardized cutaneous activity measurements decreased at follow up, though damage measures were unchanged (Table 1). At baseline, 4/5 patients had facial asymmetry RMSD exceeding 2 standard deviations (SD) of normal and 2/5 exceeded 3 SDs. All patients had facial asymmetry RMSD >2SD at the end of the follow-up period (28 months), and 4/5 exceeded 3 SDs. Asymmetry increased in 80% (4/5) compared to baseline (Table 2, Figure 1).
Conclusion: Facial asymmetry in patients with craniofacial scleroderma is reliably detectable by 3D stereophotogrammetry. Asymmetry generally worsens over time. BMI and age-related skeletal growth do not appear to influence asymmetry. Conventional cutaneous scoring may fail to detect relevant changes in damage the lead to progressive asymmetry.
 Figure 1. Longitudinal facial asymmetry root mean square deviation (RMSD) values. Baseline and four follow up time points are denoted. The dashed line represents the upper limit of normal RMSD values (1.28mm), defined as 2 standard deviations (0.24mm) above the normative mean (0.80mm) per Taylor et al 2014.
Figure 1. Longitudinal facial asymmetry root mean square deviation (RMSD) values. Baseline and four follow up time points are denoted. The dashed line represents the upper limit of normal RMSD values (1.28mm), defined as 2 standard deviations (0.24mm) above the normative mean (0.80mm) per Taylor et al 2014.
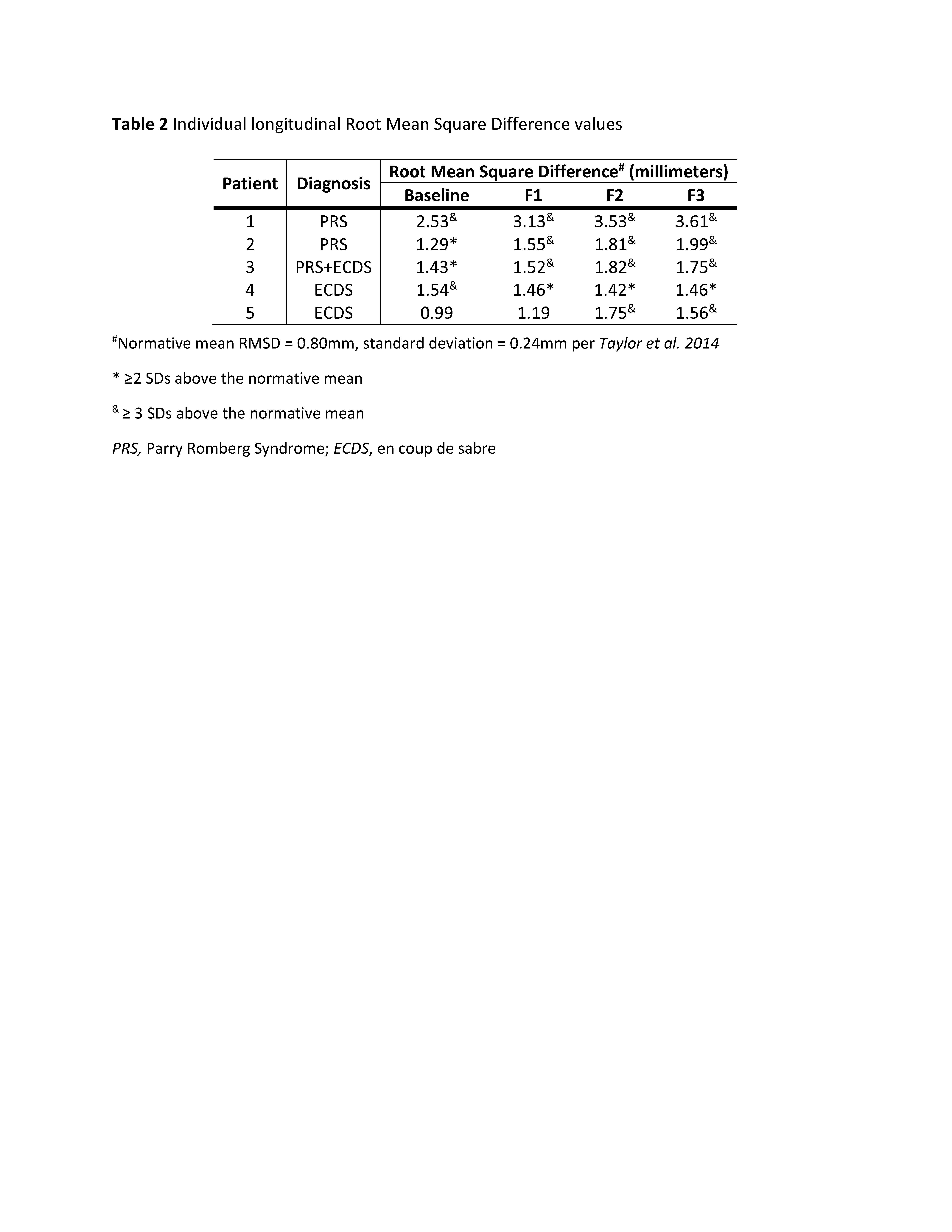 Table 2 Individual longitudinal root mean square difference values
Table 2 Individual longitudinal root mean square difference values
To cite this abstract in AMA style:
Glaser D, Liu C, Torok K. Three-Dimensional Analysis of Facial Asymmetry in Craniofacial Scleroderma [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/three-dimensional-analysis-of-facial-asymmetry-in-craniofacial-scleroderma/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/three-dimensional-analysis-of-facial-asymmetry-in-craniofacial-scleroderma/