Session Information
Session Type: Abstract Session
Session Time: 10:00AM-10:50AM
Background/Purpose: Infection can trigger coagulation pathways and increase the risk of thrombosis. However, the impact of infection on postoperative venous thromboembolism (VTE) risk is poorly defined. The aim of this study was to assess the 90-day risk of VTE following total knee replacement (TKR) revision by indication for revision to estimate the impact of infection on postoperative VTE risk.
Methods: We used New York Statewide Planning and Research Cooperative System data to identify all New York State residents undergoing TKR revision from 1998 to 2014. Only the first revision was included for patients undergoing multiple revisions. ICD-9-CM codes were used to identify patient comorbidities and classify indication for TKR revision as aseptic, septic or fracture. The primary outcome was any diagnosis code for VTE (pulmonary embolism and/or deep vein thrombosis) recorded for the revision surgery and/or subsequent admissions within 90 days. A multivariable logistic regression analysis adjusting for demographics and comorbidities was performed to estimate the risk of VTE after septic vs aseptic revision TKR, and of fracture-related revision vs. aseptic revision.
Results: This study included 25,441 TKR revision surgeries, 17,563 (69%) of them aseptic, 7075 (28%) septic and 803 (3%) for fracture. Mean (SD) age was 66 (12) years, 15,592 (61%) were female, 3198 (12%) were black, 1192 (5%) were smokers and 4222 (17%) were obese (Table 1). A total of 719 (2.8%) patients experienced VTE within 90 days of revision TKR, 387 (1.5%) during the index admission. The 90-day incidence of VTE was 2.1% after aseptic revision, 4.3% after septic revision and 5.9% after revision for fracture (Table 2). The 90-day incidence of pulmonary embolism was 0.7% after aseptic revision, 1.0% after septic revision and 1.9% after revision for fracture. The adjusted odds ratio (OR) for VTE relative to aseptic revision was 2.01 (95% CI 1.72-2.36) for septic TKR revision and 2.61 (95% CI 1.9-3.58) for fracture-related TKR revision (Table 3). Prior history of VTE was also a risk factor for post revision VTE (OR 2.01, 95% CI 1.48-2.71, p< 0.001).
Conclusion: The risk of VTE after septic TKR revision is double that after aseptic TKR revision. Although fractures account for a small percentage of TKR revisions, the risk of VTE is 2.6-fold higher after those procedures. VTE prophylaxis guidelines should distinguish between the indications for TKR revision, and potent/fast acting VTE prophylaxis should be strongly considered in those with infection or fracture.
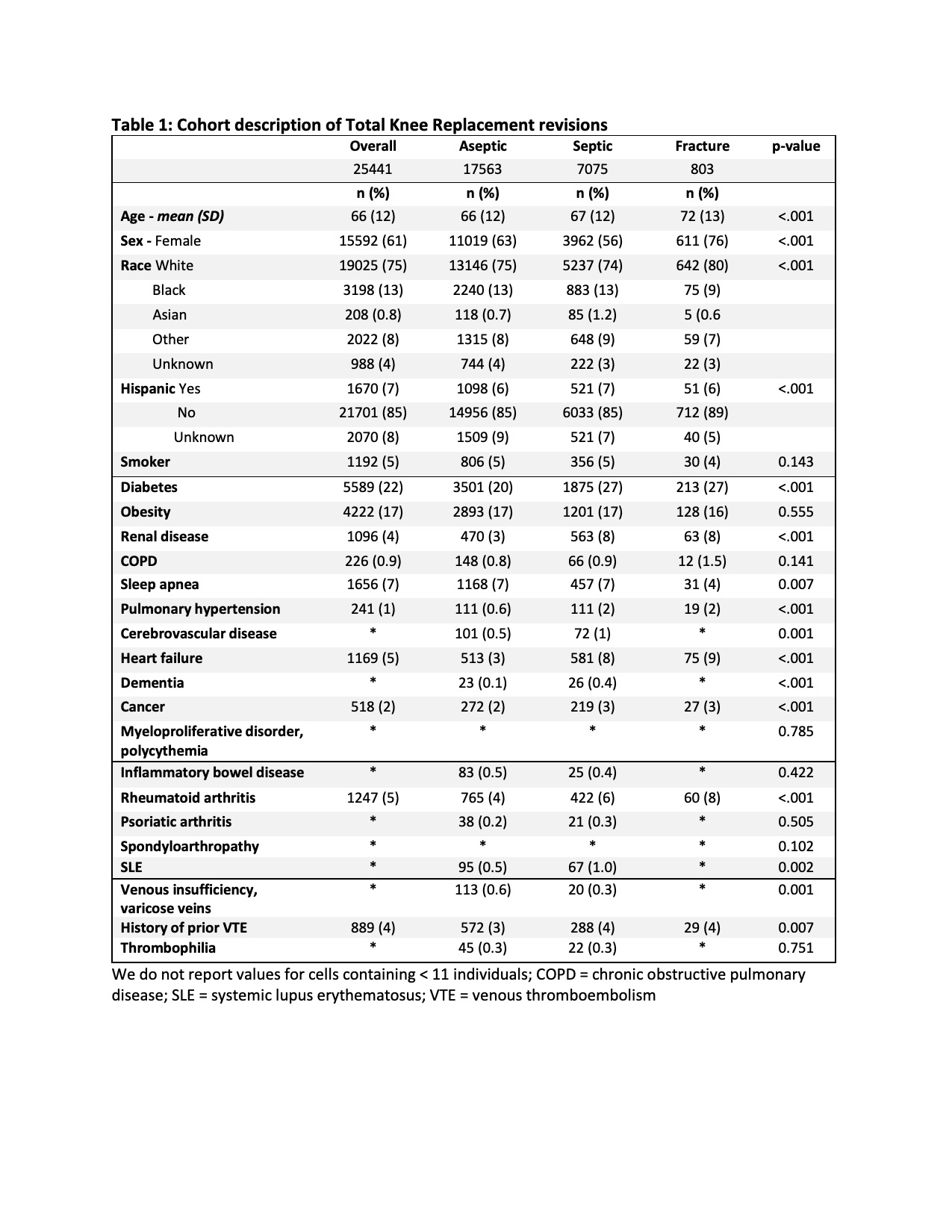 Table 1: Cohort description of Total Knee Replacement revisions
Table 1: Cohort description of Total Knee Replacement revisions
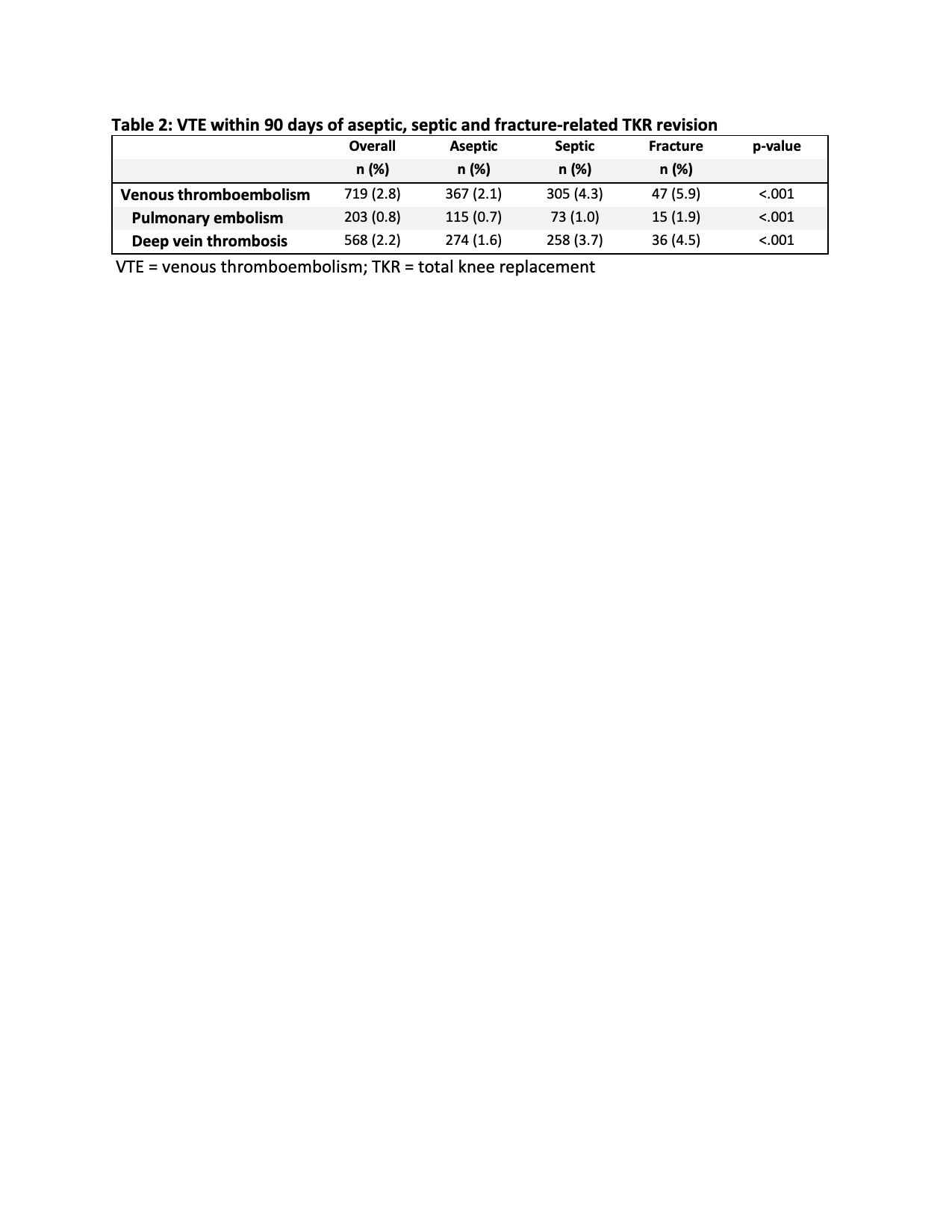 Table 2: VTE within 90 days of aseptic, septic and fracture-related TKR revision
Table 2: VTE within 90 days of aseptic, septic and fracture-related TKR revision
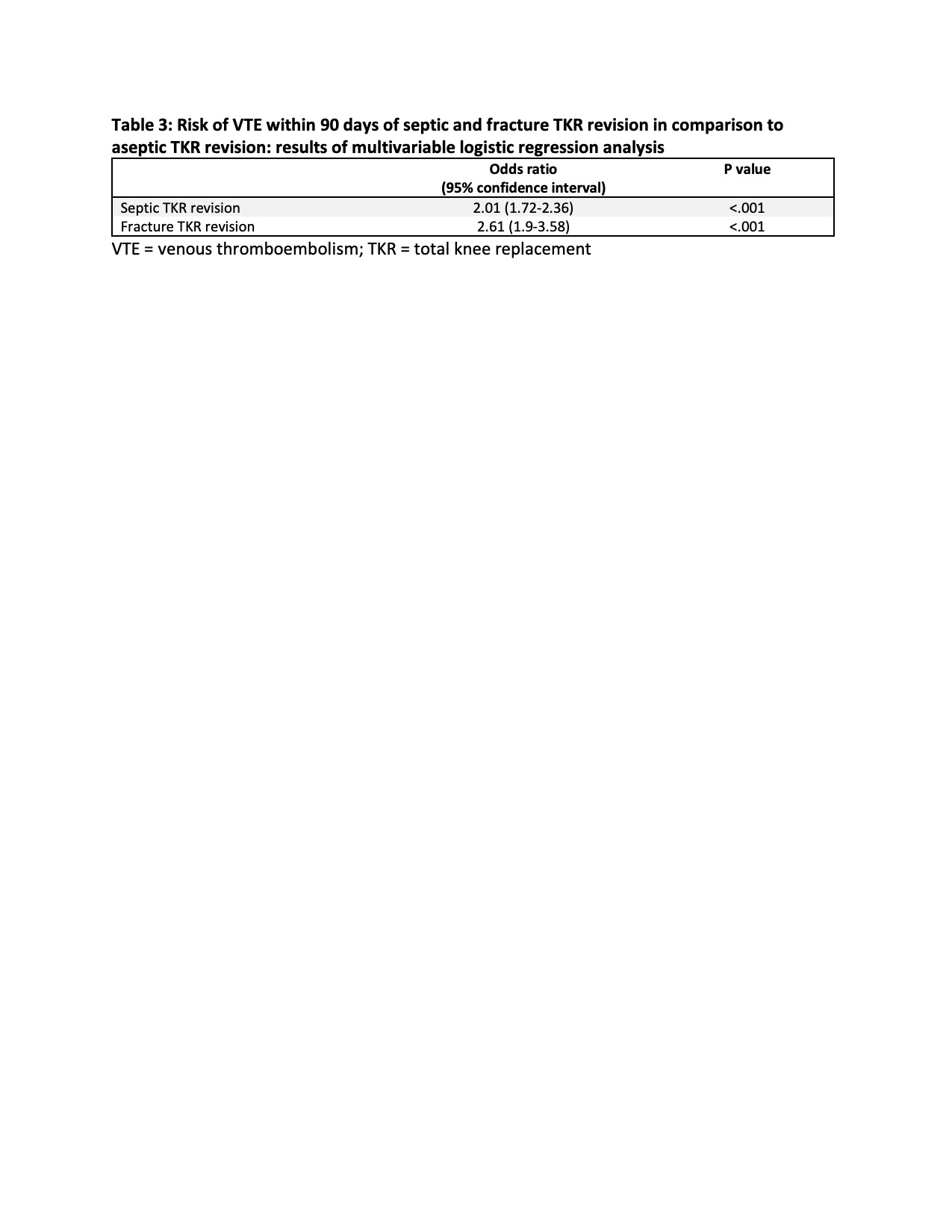 Table 3: Risk of VTE within 90 days of septic and fracture TKR revision in comparison to aseptic TKR revision: results of multivariable logistic regression analysis
Table 3: Risk of VTE within 90 days of septic and fracture TKR revision in comparison to aseptic TKR revision: results of multivariable logistic regression analysis
To cite this abstract in AMA style:
Bass A, Mehta B, Sculco P, Zhang Y, Do H, Russell L, Goodman S. The Risk of Venous Thromboembolism After Septic Total Knee Replacement (TKR) Revision Is Double the Risk After Aseptic TKR Revision: An Analysis of Administrative Discharge Data [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/the-risk-of-venous-thromboembolism-after-septic-total-knee-replacement-tkr-revision-is-double-the-risk-after-aseptic-tkr-revision-an-analysis-of-administrative-discharge-data/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-risk-of-venous-thromboembolism-after-septic-total-knee-replacement-tkr-revision-is-double-the-risk-after-aseptic-tkr-revision-an-analysis-of-administrative-discharge-data/
