Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose:
Systemic sclerosis (SSc) is associated with several risk factors for osteoporosis and fractures due to malabsorption or malnutrition, physical disability, chronic inflammation, and use of corticosteroid therapy. However, the risks for osteoporosis and fracture in SSc patients in the United States not well-defined. The aim of this study was to examine the relationship between risk factors (e.g. medication use, clinical characteristics of SSc) and the incidence of fractures and osteoporosis (OP) in SSc patients in a large U.S. cohort.
Methods:
Patients from 1998 to 2019 in FORWARD, National Databank for Rheumatic Diseases, were screened. Patients with SSc and respective 5:1 age- and gender-matched patients with osteoarthritis (OA) from the same database were included as controls. The primary endpoint was the occurrence of a physician-confirmed diagnosis of OP or an osteoporotic fracture. Single and multivariate Cox proportional hazard models were used to investigate the risk factors for fractures or OP in the SSc and OA cohorts. Models were constructed using stepwise and purposeful selection methods.
Results:
The study included 922 patients, 154 with SSc and 768 with OA. For 5046 patient-years (median (IQR) 4.16 (6.2)) of follow-up, 90 patients had either a fracture or incident OP. Univariate analysis (Table 2) showed a significant fracture/OP risk (HR (95% CI)) increase for women (HR 2.49 (1.09 – 5.71)), with being underweight (HR 4.57 (1.56 – 13.4)), higher rheumatic disease comorbidity index (HR 1.10 (1.07 – 1.39)), higher Health Assessment Questionnaire Disability Index (HAQ) (HR 1.60 (1.16 – 2.20)), proton pump inhibitor (PPI) use (HR 1.62 (1.05 – 2.47)), SSRI use (HR 1.91 (1.15 – 3.18)), and OP medication use (HR 2.08 (1.10 – 3.94).
The adjusted model (Table 3) of the combined cohort showed a significant increase in fracture/OP risk with PPI use (HR 1.58 (1.01 – 2.49)), higher HAQ score (HR 1.48 (1.00 – 2.50)), and with being underweight (HR 5.37 (1.69 – 17.0)). However, in the subgroup analysis of SSc patients, PPI use was associated with lower risk (HR 0.81 (0.29 – 2.29)), with the lower risk being significant for those with the highest cumulative omeprazole-equivalent PPI exposure (HR 0.15 (0.03 – 0.85).
Conclusion:
Our findings suggest that several risk factors are associated with a higher risk of fractures in SSc. Functional status of SSc and OA patients, as measured by HAQ, is a particularly strong indicator of future fracture/OP risk. Thus, interventions aimed at improving patients’ functional status may lead to improved clinical outcomes. Furthermore, while PPIs are often associated with a higher risk of fractures/OP, our findings suggest that such risks may vary across different disease types. Further investigations are necessary to further characterize these relationships.
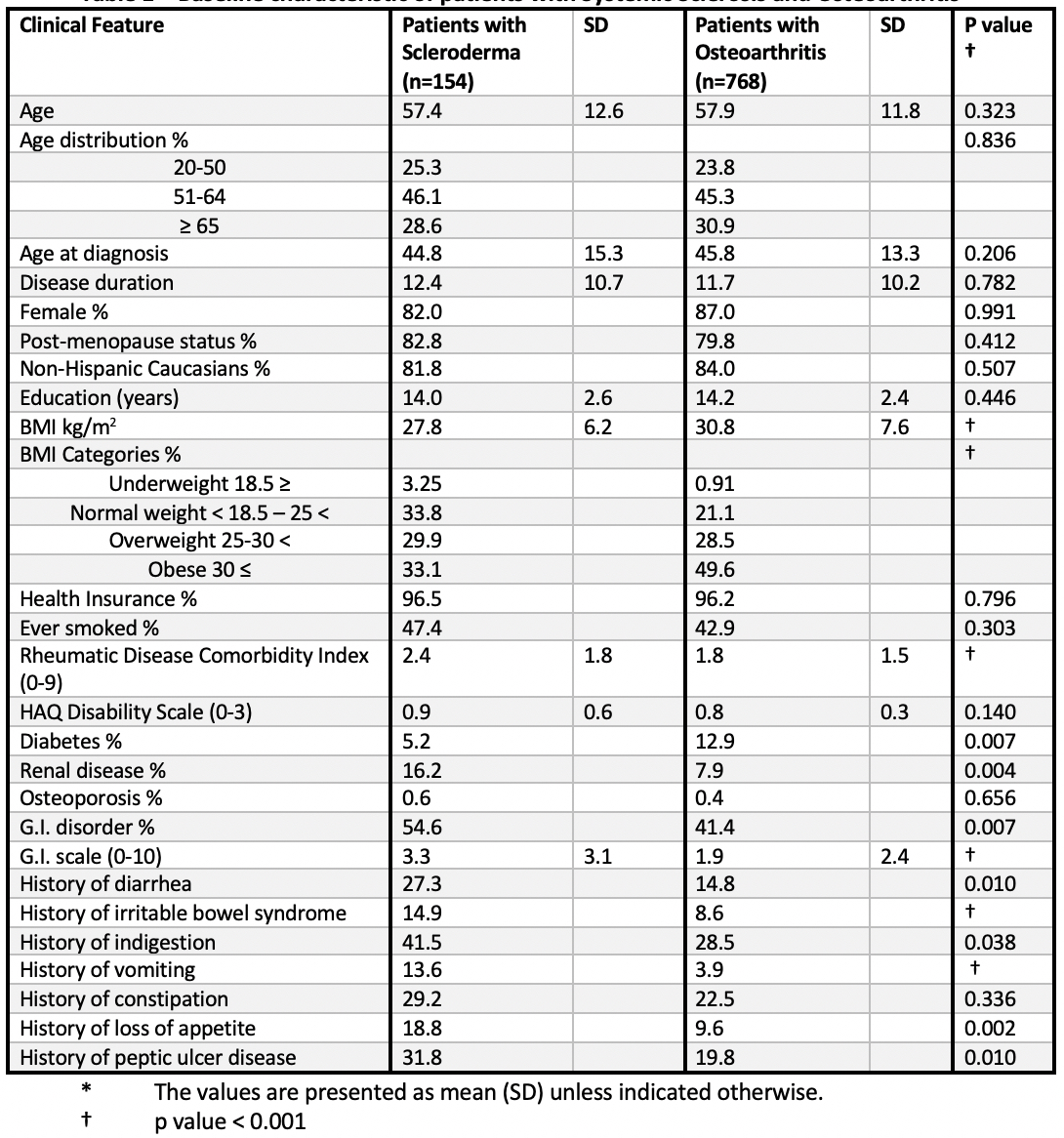 Table 1 – Baseline characteristic of patients with Systemic Sclerosis and Osteoarthritis
Table 1 – Baseline characteristic of patients with Systemic Sclerosis and Osteoarthritis
 Table 2. Univariate Risk Factor Analysis of Fractures and Osteoporosis (OP) in Patients with SSc and OA
Table 2. Univariate Risk Factor Analysis of Fractures and Osteoporosis (OP) in Patients with SSc and OA
 Table 3. Multivariate Risk Factor Analysis of Fractures and Osteoporosis (OP) in Patients with SSc and OA
Table 3. Multivariate Risk Factor Analysis of Fractures and Osteoporosis (OP) in Patients with SSc and OA
To cite this abstract in AMA style:
Famenini S, Perin J, Wipfler K, Michaud K, McMahan Z. Risk Factors for Fractures and Osteoporosis Among Patients with Systemic Sclerosis in a United States Cohort [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/risk-factors-for-fractures-and-osteoporosis-among-patients-with-systemic-sclerosis-in-a-united-states-cohort/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-factors-for-fractures-and-osteoporosis-among-patients-with-systemic-sclerosis-in-a-united-states-cohort/
