Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Lupus nephritis (LN) contributes to a 10-fold higher risk to develop kidney failure and 26-fold higher mortality compared to peers. Kidney biopsy remains a gold-standard to diagnose LN and start therapy. Yet, our prior study highlighted that the average wait time to see a specialist and undergo a kidney biopsy was >50 days, with no change over 20 years (1997-2017). Further, studies report that high-impact quality process measures, such as ACE inhibitors use and addressing social needs, are often missed during routine SLE visits, contributing to poor LN outcomes. Therefore, we implemented a multidisciplinary LN clinic to provide targeted strategies to overcome such barriers to improve care and LN outcomes. We aimed to examine time to biopsy and quality measures provided to LN patients before and after the implementation of LN clinic.
Methods: All validated adult LN patients with diagnostic kidney biopsy preformed between 2011-2020 were identified from our comprehensive native kidney biopsy database at an academic center. Data on sociodemographic, disease characteristics and biopsy date were abstracted from this database. We manually abstracted data on medications, date of abnormal labs or LN specialist referral, vaccinations and social needs to examine quality process measures. Time to biopsy was defined as time from abnormal labs or LN specialist referral until biopsy. Pre- and post-LN clinic period included patients who underwent biopsies between 2011-2017 and 2018-2020, respectively. We used KM analysis to compare time to biopsy during the two periods, and Cox Proportional hazards models to examine predictors of time to biopsy. We used Fisher and two-sample t-tests to compare socio-demographics and quality measures during these two periods.
Results: The pre-LN clinic period included 53 LN patients, the mean age was 36 years, 75% were female and 74% were white (Table 1). During the post-LN clinic period, 21 LN patients underwent diagnostic biopsy. The mean age was 35.6 years, 62% were female and 51% were white.
The mean and median time to biopsy in the pre-LN clinic period were 202 and 26 (IQR 7-120) days, and during the post-LN clinic period were 22 and 16 (IQR 8-21) days. The median time to biopsy decreased by 10 days after starting the LN clinic (p 0.014; Figure 1). We found social barriers as the strongest predictor of longer wait times (HR 4.1, 95% CI 1.2-12, p 0.007; Table 2).
We found 13-fold higher odds of ACE inhibitors use in LN, 10-fold higher odds to complete pneumococcal vaccination, and 15-fold higher odds to address social needs during the post-LN clinic period compared to the previous period (Table 1). We noted a trend of increased hydroxychloroquine use in the post-LN clinic period.
Conclusion: This is one of the first studies to report significant improvement in wait times to diagnose LN after establishing a multidisciplinary LN clinic. Our study highlights that system and social barriers predict a delay in diagnosis, which can be addressed by including a social worker in specialized clinics. Finally, our study supports previous reports on higher quality measure performance in SLE subspecialty clinics.
 Table 1. Demographics of Adult LN Patients During Pre- and Post-LN Clinic Periods
Table 1. Demographics of Adult LN Patients During Pre- and Post-LN Clinic Periods
 Figure 1. KM Plot: Time to Outpatient Biopsy Pre (2011-17) & Post (2018-20) LN Clinic
Figure 1. KM Plot: Time to Outpatient Biopsy Pre (2011-17) & Post (2018-20) LN Clinic
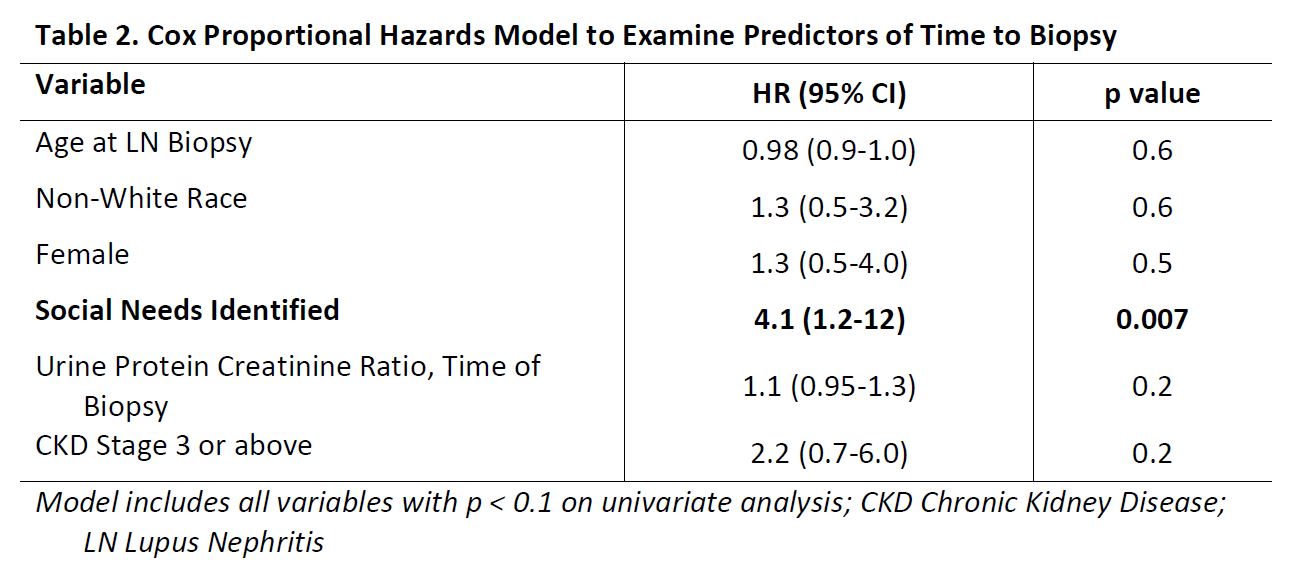 Table 2. Cox Proportional Hazards Model to Examine Predictors of Time to Biopsy
Table 2. Cox Proportional Hazards Model to Examine Predictors of Time to Biopsy
To cite this abstract in AMA style:
Garg S, Plafkin C, Singh T, Panzer S, Bartels C. Impact of a Dedicated Lupus Nephritis Clinic to Improve Time to Biopsy and Care Quality [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/impact-of-a-dedicated-lupus-nephritis-clinic-to-improve-time-to-biopsy-and-care-quality/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-a-dedicated-lupus-nephritis-clinic-to-improve-time-to-biopsy-and-care-quality/
