Session Information
Date: Saturday, November 7, 2020
Title: Epidemiology & Public Health Poster II: OA, Osteoporosis, & Other Rheumatic Disease
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Foot osteoarthritis (OA) is a common cause of disability in older adults yet remains an understudied area. The purpose of this study was to examine the incidence and progression of foot osteoarthritis (OA), as well as potential risk factors, in a large population-based cohort.
Methods: Data were from the Johnston County Osteoarthritis Project (JoCoOA), a prospective population-based cohort of African American and White adults. Participants completed foot radiographs at baseline (2013-2015) and follow-up (2016-2018), which were scored using the La Trobe Foot Atlas to examine osteophytes (OP, score 0-3) and joint space narrowing (JSN, score 0-3) in the first metatarsophalangeal (1st MTP), first cuneometatarsal (1st CMT), second cuneometatarsal (2nd CMT), naviculocuneiform (NC), and talonavicular (TN) joints. Incident foot radiographic OA (rOA) was defined as baseline score < 2 OP and JSN in all 5 joints with ≥2 OP or JSN at follow-up in any of the 5 joints. Progression was defined as worsening score of OP or JSN in a joint with baseline foot rOA. At baseline and follow-up, participants were asked to rate their pain, aching, or stiffness [PAS] in each foot as 0-10 (none to extreme) on most days of any month in the past 12 months. PAS worsening was defined as an increase in the PAS from baseline to follow-up. The Foot and Ankle Outcome Score (FAOS) (pain, other symptoms, activities of daily living [ADL], sport and recreation function [Sports & Rec], foot and ankle-related quality of life [QOL]) was also obtained at both time points. Joint-based logistic regression models with generalized estimating equations were used to examine associations of foot rOA incidence and progression and covariates of interest (Table 1). Two-way interactions between risk factors and foot rOA status at baseline were assessed at a 0.10 alpha level and adjusted odds ratios and 95% confidence intervals (aOR [95% CI]) were shown by baseline status if significant; otherwise overall associations were reported.
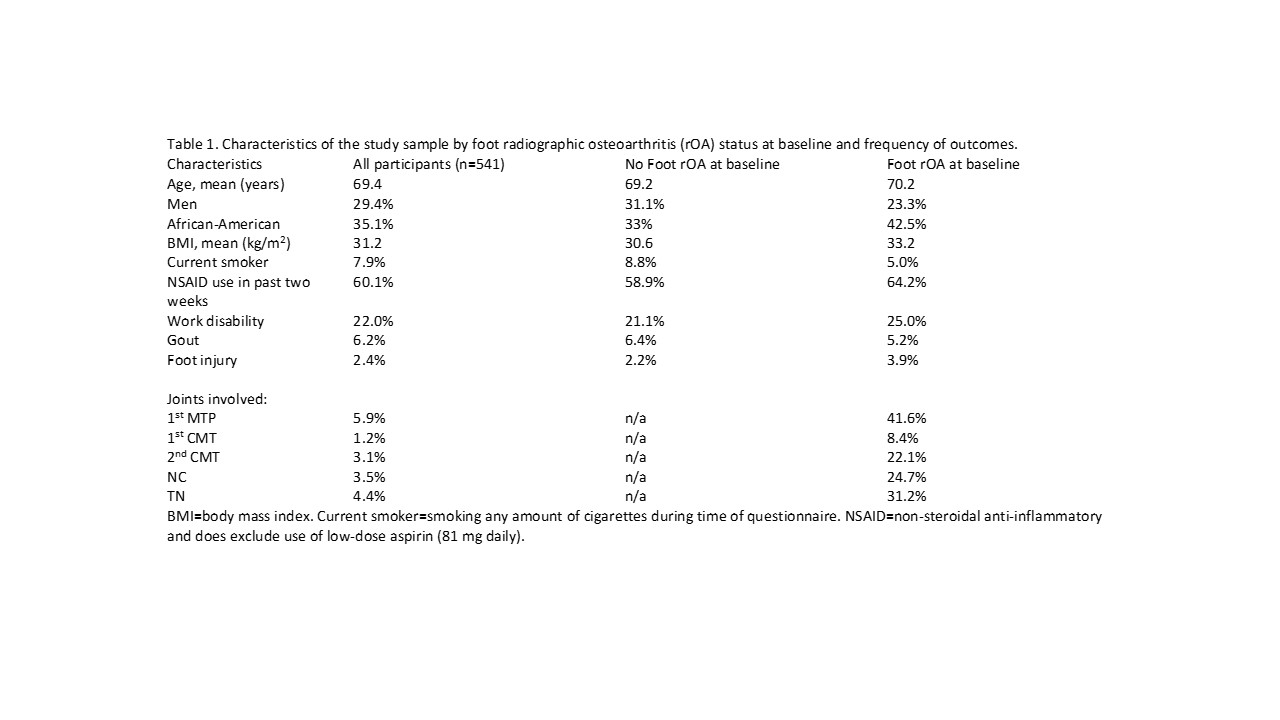
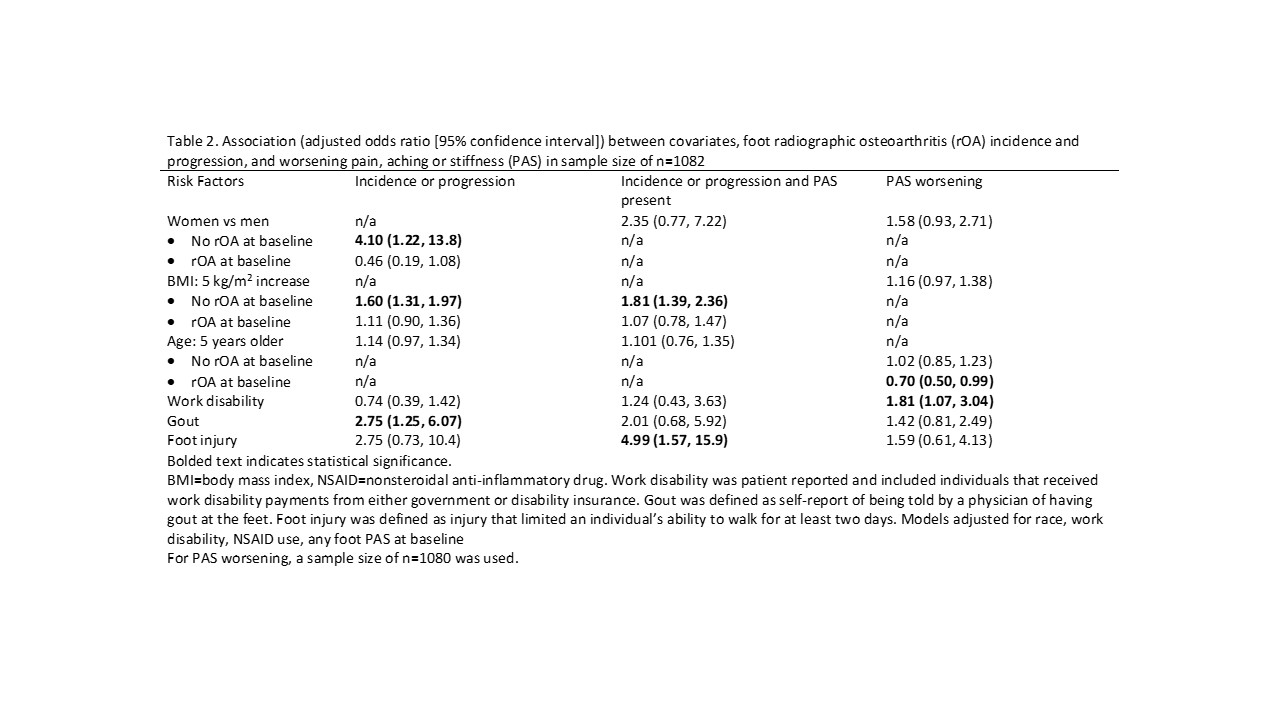
Results: A total of 541 participants (1082 feet) were included (71% women, mean age 69 years; 35% African American, 53% obese; Table 1). Among 928 feet without baseline rOA, 4% developed incident foot rOA and roughly 2% of those had PAS of the same foot at follow-up (Table 1). Among 154 feet with baseline foot rOA, 55% had radiographic progression and 16% of those had PAS of the same foot at follow-up. Female sex and higher BMI were associated with incident foot rOA, while history of gout was associated with both incidence and progression of foot rOA (Table 2). History of foot injury was associated with foot OA with PAS present. Work disability was associated with PAS and FAOS worsening particularly for pain, ADL, and Sports & Rec subscales (Table 3). BMI was associated with worsening of all FAOS subscales, and history of gout was associated with worsening for FAOS ADL and Sports & Rec subscales.
Conclusion: Progression of foot rOA is relatively common, although it is not necessarily related to worsening symptoms. Given the increased risk of foot OA outcomes with higher BMI, foot injury, and history of gout, further studies could examine interventions (e.g., weight loss, injury prevention, intensive gout control) to reduce or manage foot OA.
To cite this abstract in AMA style:
Eltaraboulsi R, Nelson A, Alvarez C, Renner J, Bowen C, Gates L, Golightly Y. Incidence and Progression of Foot Osteoarthritis [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/incidence-and-progression-of-foot-osteoarthritis/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/incidence-and-progression-of-foot-osteoarthritis/