Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Interstitial lung disease (ILD) is the leading cause of death in patients with systemic sclerosis (SSc). Although pulmonary function tests (PFTs) are commonly used to screen for ILD in patients with SSc, studies have shown that they lack sensitivity for the detection of ILD. Moreover, although high resolution computed tomography (HRCT) scan of the chest is the gold standard test for detection of ILD, there is no consensus among rheumatologists regarding the use of HRCT to screen for ILD in their SSc patients. The aims of this study were to describe the HRCT ordering practices at expert SSc centers in the US, and to determine which patient characteristics are associated with HRCT ordering.
Methods: We performed a retrospective cohort study of patients enrolled in the Collaborative National Quality and Efficacy Registry (CONQUER) at 13 sites in the US between June 6, 2018, and February 1, 2020. CONQUER is a US-based, multicenter cohort of adults with SSc who met 2013 ACR/EULAR Classification Criteria and had a disease duration ≤5 years from the 1st non-Raynaud’s symptom at enrollment. We used the Student’s t test, chi square test, and Fisher’s exact test, as appropriate, to compare baseline characteristics between participants who did and did not undergo HRCT. We performed univariate logistic regression (LR) followed by multivariable LR to determine which patient characteristics were associated with HRCT ordering. Each variable that attained a p-value< 0.1 in the univariate analysis was included in the final multivariable LR model, as were age and sex. Statistical significance in the univariate and multivariable models was defined as a p-value< 0.05.
Results: 356 SSc patients were enrolled in CONQUER, of whom 285 (80%) underwent HRCT at some point during their SSc disease course. Among those who underwent HRCT compared to those who did not, a smaller proportion were centromere positive (9.5% vs. 22.5%) and a greater proportion had crackles on exam (23.5% vs. 9.9%). SSc patients who underwent HRCT had lower forced vital capacity (FVC), forced expiratory volume in 1 second (FEV1), and diffusion capacity for carbon monoxide (DLCO) than those who did not (Table 1). In univariate analyses, the following variables were statistically significantly associated with HRCT ordering: crackles on pulmonary exam, FVC< 80%, FEV1< 80%, total lung capacity (TLC)< 80%, missing TLC%, and DLCO< 60% (Table 2). A positive centromere antibody was negatively associated with HRCT ordering. In the final multivariable LR model, positive centromere antibody remained negatively associated and missing TLC% remained positively associated with HRCT ordering (Table 3).
Conclusion: 80% of SSc patients enrolled in CONQUER at 13 expert SSc centers in the US underwent HRCT. Abnormal PFTs and crackles were associated with HRCT ordering in univariate analyses. However, in the multivariable analysis, only a positive centromere antibody remained associated with a decreased odds of HRCT ordering and a missing TLC% remained associated with an increased odds of HRCT ordering. Given the poor sensitivity of PFTs for the detection of SSc-ILD, research is needed about how to increase rheumatologists’ HRCT ordering practices in their SSc patients.
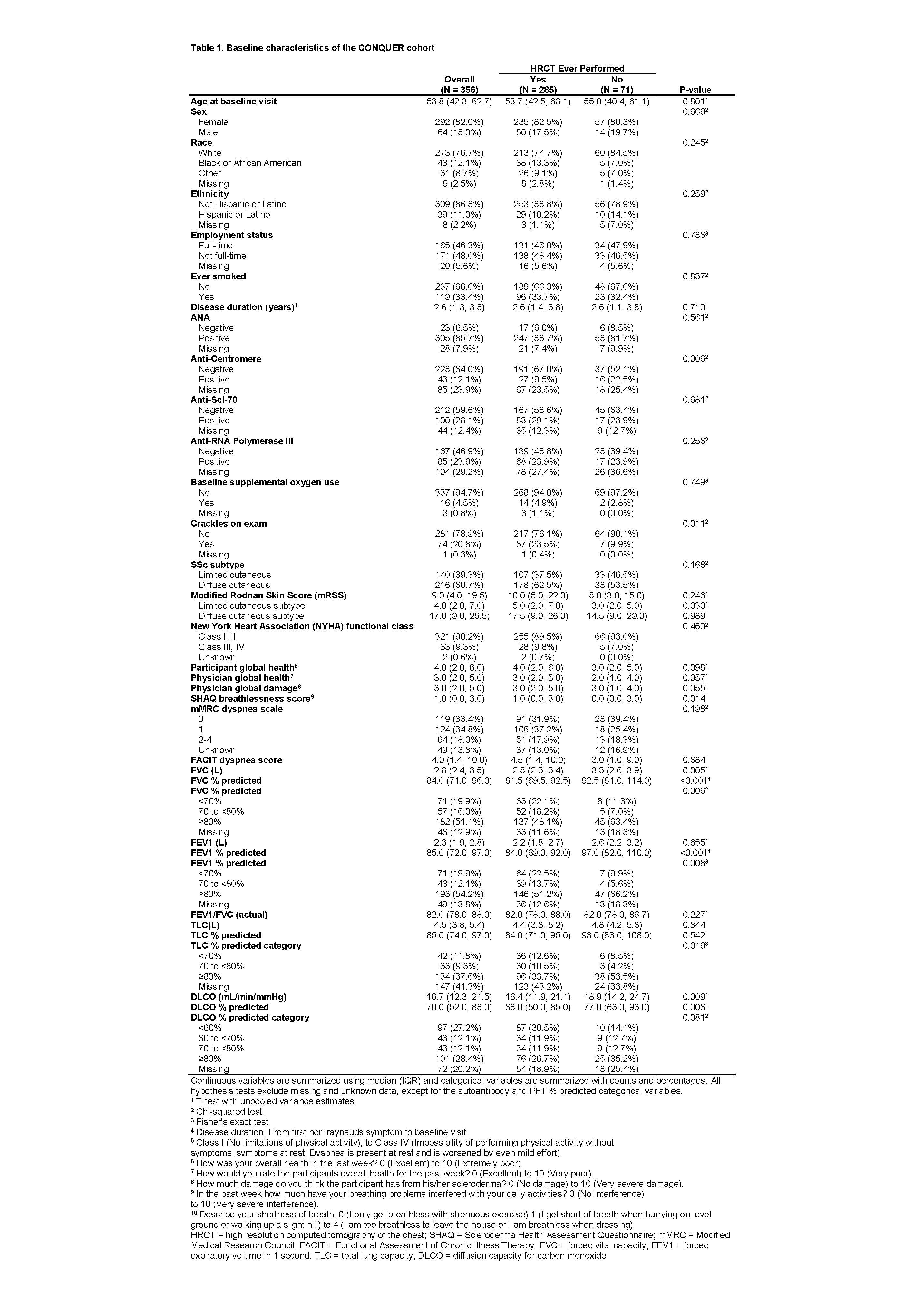 Table 1: Baseline characteristics of the CONQUER cohort
Table 1: Baseline characteristics of the CONQUER cohort
To cite this abstract in AMA style:
Bernstein E, VanBuren J, Assassi S, Castelino F, Chung L, Correia C, Evnin L, Frech T, Startup E, Gordon J, Hant F, Hummers L, Sandorfi N, Shah A, Shanmugam V, Steen V, Khanna D. Chest CT Ordering Practices at Expert Scleroderma Centers in the United States [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/chest-ct-ordering-practices-at-expert-scleroderma-centers-in-the-united-states/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/chest-ct-ordering-practices-at-expert-scleroderma-centers-in-the-united-states/


